On this blog, we frequently write about what it’s like to work for — or experience life at — Penn Medicine. What we don’t get the chance to write about very often is what it’s like to see the University of Pennsylvania Health System from the other side: as a patient, just trying to figure out what’s wrong and get better. Fortunately (well, not ‘fortunately,’ per se, but you get the idea), I’ve now got one such story to relate. This is the third and final part.
MR Arthrogram (or: Sound and Fury)
Years and years ago (around 1994), I was sitting on my bed playing Aladdin for the Sega Genesis when I noticed I was having trouble seeing the screen. It was like a blind spot near the middle of my visual field, a distortion or void that my mind tried ineffectually to fill in with nearby colors.
I was experiencing my very first visual aura — a precursor to my very first migraine.
I get migraines to this day, and with rather startling frequency. I’ve seen I don’t even know how many doctors about ‘em over the years, and the very first thing they all do is order an MRI. That’s standard procedure, as far as I’m aware, but it also means my very first migraine was followed quite closely with my very first MRI.
I’m going to nerd out about how an MRI works for a little bit, so if you don’t really care, just skip the next paragraph or two. MRI stands for “magnetic resonance imaging,” and, as the name implies, relies on the use of large magnets. Hydrogen makes up about three-quarters of all the mass in the universe, and about ten percent of your body mass. Each hydrogen atom has one proton — and therein lies their importance here, because a proton is essentially a very (very, very) tiny magnet. By running your body under, over, through, or near a giant magnet, we can make all of those protons line up in the same direction. Hitting those protons with radio waves knocks them out of alignment, and their ensuing realignment creates radio signals. Those radio signals get picked up by receivers in the machine, and suddenly we’ve got a detailed image of the inside of the human body.
Consider for a second how bonkers it is that we, as a species, even figured out we could do that. The first transatlantic phone call happened in 1927. The first MRI was performed in 1977. In the span of just fifty years, we went from being amazed at the concept of ringing someone in London all the way to figuring out we could play with the alignment of your body’s atomic building blocks to get a better picture of whatever’s going on in there.
So, anyway, MRIs: I’ve had a bunch of them. I know the score. As I’m in a small room off to the side of the machine itself waiting for my turn, one of the techs comes over and talks to me a bit about the procedure.
“Do you have any sort of metal in your body? Implants, screws, rods, shunts, a pacemaker … ?” she asks. It’s at least the fifth time today someone’s thrown the question out there. I can’t help but snicker as I say no, no there is not. She asks again, because I guess snickering the first time made it look like I was trying to pull a fast one. I say no, this time with the straightest face I can muster.
It’s an important question. As you might imagine, metal and MRI machines are not great partners. Or, more accurately, they’re incredible partners that you can’t allow to occupy the same room. Here’s a fun little video showing the sort of power the magnets we’re talking about actually have, produced by some folks who basically have my dream job:
The tech goes through a few basics, then walks me over to the room with the MRI machine itself. The entrance of the room is guarded by two large, lit posts, one on either side. There’s also some cautionary signage on the floor. The real feature, however, is the door. It’s huge. Like, bank vault huge. It swings aside a little and I’m able to view the 13-ton MRI machine in its full glory.
It’s basically a large, eggshell-white rectangle with a hole in the middle. Sticking out of the hole is a table, upon which the patient is placed and then wheeled inward. The whole contraption takes up a huge chunk of the room, and I cast an eye back to the door.
“That’s not really gonna stop the sort of person walking out of here with this machine,” I think to myself.
The tech ushers me onto the table and begins some basic setup, which mostly involves positioning me and my legs so the clearest and most useful images can be obtained.
“It’s going to be about twenty, twenty-five minutes,” she tells me. “You need to stay completely still. You’ll probably feel a little warmth as the machine works. It’s also going to be really loud, so we’re going to give you earplugs.”
I’m offered music, but decline. The tech does one final pass to make sure I’m comfortable — an uncomfortable patient’s not going to be staying perfectly still for twenty-five minutes — then hands me the earplugs and walks out of the room. The earplugs are maybe a little too effective, because once the tech is at her station and communicating with me through the intercom, I realize I’m only just barely able to hear her when she says they’re going to get started.
I feel the table start to move underneath me, and slowly I slide into the machine. When I was getting my very first MRI at the age of eight, this was terrifying. Now, though? Can’t say I’m terrified. More fascinated. Maybe a little itchy.
One thing they really can’t prepare you for, much as they might try, is just how loud the machine actually is. It’s one of those things that you know is working if it sounds broken. Loud bangs, clangs, buzzes, and hums fill the air around me, and I’m grateful for my earplugs. After a while, a pattern starts to emerge. It feels a little like when you hear a car alarm for so long that you start attributing a voice to it.
The next twenty-five minutes pass somewhat quickly, and very uneventfully. The warmth the tech said I’d notice does, in fact, show up, but it’s barely noticeable — especially in comparison to the still oddly full feeling my newly injected hip is generating. The tech’s barely audible voice comes over the intercom to let me know they’re done with this set of images, and soon I’m repositioned for another set. It takes about the same amount of time as the first.
“You did great!” the tech says as I’m allowed to get off of the table, and for a second I’m filled with pride at my ability to stay perfectly still and do nothing whatsoever. “You’re free to go. You can get changed, and they’ll want to make an appointment with you at the front desk on your way out.”
I get changed and make my way out to the front desk, where I set an appointment in a week’s time with the orthopedic doctor.

Finally, Results (or: Ayup, that’s Your Problem Right There)
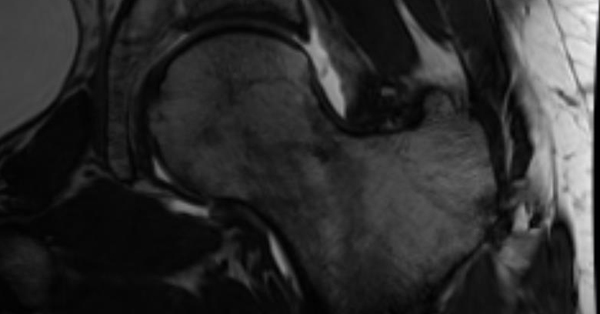
It’s a week later, and I’m waiting in the office of the doctor who first sent me down this road several weeks before. The images that were taken the week previously — X-ray and MRI alike — have been brought up onto the monitor for the doctor’s perusal. I’m looking at them and suddenly feeling self-conscious, because one thing the MRI shows very effectively is a nice layer of fat. I try to ignore that and pick out the troubled part of the joint. It does feel good to know I’m about to get some answers.
There’s a quick knock at the door. Just as he did the first time around, the doctor opens it quickly and sweeps into the room, white coat trailing him with just a little bit of majesty.
“Hello again,” he says cheerfully as he sits down. “How are you feeling?”
I tell him I’ve actually been feeling pretty okay — which I have — and he nods as he scrolls through the images on the screen.
He stops at one image that looks, to me, like just about every other image. I’m still trying to figure out which way the joint’s even facing when he gestures for me to move in closer and points to a small white-ish spot on the screen. He tells me that’s where the contrast fluid managed to make it through the labrum. I’m reminded of when I go to the mechanic and he brings me into the garage. Yeah, see that? You uh, you got a busted flange there. You’re gonna need a new flange. A new flange and maybe a new gasket. We’ve got one in the back, but it’s not gonna be cheap.
The fluid leaking through the labrum, he explains, is indicative of an injury. There are a few points of concern, in fact, and he scrolls through some of the images to show me how different cross-sections of my hip display different levels of tearing. Long story short: It’s pretty much exactly what we thought it was.
“Well, okay,” I say. “What’s the next step?”
Quick flashback: About three years into college, I managed to mess up my shoulder. It required an MRI — as these things are wont to do — and resulted in a conversation with my doctor at the time that went just about the same as the conversation I was about to have with the doctor in front of me.
See, the shoulder and the hip are similar in the sense that neither area gets particularly good blood flow. A lack of decent blood flow means those areas aren’t all that great at healing themselves. I got away with not having my shoulder operated on, but my hip’s not likely to be so forgiving. It’s likely to keep bothering me whenever it gets disturbed. Think of it like a hangnail: If you’re not pushing or hitting it against something, you might not notice it — but then you do, and it makes itself very noticeable.
Much like with a hangnail, the only way to really deal with that is to fix it directly.
“So,” I say, “I need to get it operated on?”
The doctor looks at the images, then looks at me. His eyebrows are raised, his lips lowered. He folds his fingers in front of him and sits back in his chair. He then tells me that if this injury isn’t impacting my daily activities, isn’t causing me much pain, and isn’t keeping me from doing what I want to do, he doesn’t see it as necessary.
The look on my face probably tells him I wasn’t expecting that sort of answer, and he continues by telling me that there’s a certain lack of urgency because this isn’t something critical like cancer or appendicitis. It’s mostly a quality-of-life thing.
Ultimately, it’s sort of a cost-benefit analysis: Does this injury currently bother me enough to warrant going under the knife?
The answer then, as it is now, is no. I’m actually doing pretty well. I’ve still got a full range of motion. I don’t jog anymore, but there’s plenty of other cardio to be done and I always hated jogging anyway (thanks to a bum knee, which is another old man injury for another overly long series of blog posts). Some days are worse than others, but most days are just fine with only a few minor aches and pains here and there. Like a bad roommate or a clingy friend, it’s one of those things that’s just going to be there until I finally decide I’ve had enough.
When that day comes, I guess you can expect part four not too long afterward.