 Immunotherapy once again dominated headlines during the annual meeting for the American Society of Clinical Oncology (ASCO) in Chicago, the medical conference that drew a record-breaking 35,000 oncologists and other health care professionals from the United States and around the world this year.
Immunotherapy once again dominated headlines during the annual meeting for the American Society of Clinical Oncology (ASCO) in Chicago, the medical conference that drew a record-breaking 35,000 oncologists and other health care professionals from the United States and around the world this year.
That these stories float to the top is not a surprise. Using the immune system to combat cancer has been hailed as the biggest breakthrough since chemotherapy. And data out of the meeting—some presented by researchers at Penn's Abramson Cancer Center (ACC)—continued to show that these promising therapies, both alone and with other drugs and modalities, are likely to make a powerful impact in cancer care.
"The prospect that more and more patients will be cured is becoming a reality,” Lynn Schuchter, MD, chief of Hematology/Oncology and chair of ASCO's scientific program committee for 2016, told Reuters last week in a piece that covered long-term survival results for the immunotherapy drug pembrolizumab in melanoma patients. It was one abstract among a thousand on the topic—a 20 percent increase from last year.
Of the 5,800 submitted, a fourth of the abstracts were on immunotherapy, Schuchter noted at Saturday’s special session, before introducing Robert Vonderheide, MD, Phil, associate director of translational research in the ACC, and David Porter, MD, a professor of Hematology/Oncology and director of Blood and Marrow Transplantation in the ACC. Their talks covered combination checkpoint inhibitors, so-called “immune agonists,” and chimeric antigen receptor (CAR) T cell therapies.
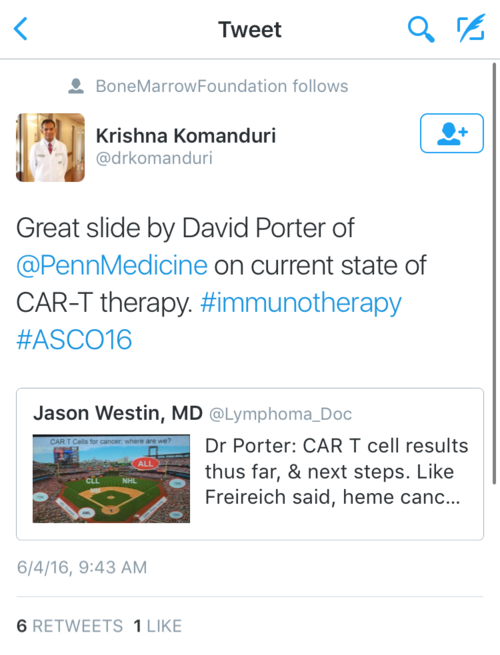
"CAR therapies will be able to overcome many limitations of chemotherapy and other immunotherapies,” said Porter, whose baseball analogy slide to illustrate the progress made in blood cancers was a hit on Twitter (acute lymphoblastic leukemia is the "home run"). “It combines the advantages of antibody therapies, cellular therapies and vaccine therapies.”
Penn’s own work with CARs was well represented at the meeting, with six CAR abstracts. Noelle Frey, MD, an assistant professor of Hematology/Oncology, presented results from the ALL trial, identifying an optimal dose and infusion regimen. “This research sought to start a conversation about maintaining high response rates while also improving tolerability, especially cytokine release syndrome,” she told HemOnc Today.
And on Monday, Joshua Bauml, MD, an assistant professor of Hematology/Oncology, presented results from a phase II clinical trial on the use of pembrolizumab in advanced head and neck cancers: 17 percent of these patients, who were left with little to no other options, partially responded to the drug, which is triple the rate seen with the standard of care.
Charu Aggarwal, MD, MPH, an assistant professor of Hematology/Oncology, who served as a discussant at Bauml’s presentation, said this trial and other trials with anti-PD-1 antibodies similar to pembrolizumab are showing meaningful responses, the ASCO Daily News reported. “Combination therapies will be required to boost response rates,” she said. “Patient selection and biomarker development are crucial. Integration of immunotherapy into earlier lines of therapy is warranted, and clinical trials are more important than ever.”
Beyond Immunity
While the meeting offered up exciting results from immunotherapy trials, one can't ignore the headway being made in other areas of cancer care, like newer approaches with targeted therapies and chemotherapies.
“We’re still treating [small cell lun g cancer patients] the same way we did 15 to 20 years ago, with very little advance” said Bauml, commenting to MedPage Today on an abstract from Memorial Sloan Kettering Cancer Center looking at the use of the targeted therapy rovalpituzumab tesirine (Rova-T). The drug stabilized disease in nearly 70 percent of the 60 evaluable patients, and 18 percent saw their tumors reduced. “It's a really exciting opportunity that we have a targeted therapy for this cancer that seems to work. My hope is that the next phases of the trials confirm these very nice responses and the toxicity profile is confirmed, so that we can have a new agent soon that we can use for this deadly disease."
g cancer patients] the same way we did 15 to 20 years ago, with very little advance” said Bauml, commenting to MedPage Today on an abstract from Memorial Sloan Kettering Cancer Center looking at the use of the targeted therapy rovalpituzumab tesirine (Rova-T). The drug stabilized disease in nearly 70 percent of the 60 evaluable patients, and 18 percent saw their tumors reduced. “It's a really exciting opportunity that we have a targeted therapy for this cancer that seems to work. My hope is that the next phases of the trials confirm these very nice responses and the toxicity profile is confirmed, so that we can have a new agent soon that we can use for this deadly disease."
Susan Domchek, MD, executive director of the Basser Center for BRCA, presented results from a Penn-involved trial looking at the use of the targeted drug rucaparib for advanced pancreatic cancer patients with a BRCA mutation. Over 30 percent saw a benefit. This “demonstrates the clinical significance of the BRCA cancer genes outside of breast and ovarian cancer, and not just in women,” Domchek said.
Treating advanced triple negative breast cancer patients with the targeted therapy CB-839 and paclitaxel also resulted in promising responses, Angela DeMichele, MD, a professor of Hematology/Oncology and Epidemiology, reported during a poster discussion presentation on Sunday. In the phase I study of 15 patients, 13 had stable disease and two had a partial response. Later on Sunday, Kara Maxwell, MD, PhD, an instructor of Hematology/Oncology, served as a discussant at a clinical science symposium for an abstract that found value using a large, multi-panel genetic test to spot mutations. Twenty-six percent of the mutations were not clinically suspected before testing, the researchers from Stanford found. Maxwell put in perspective the role of panel genetic testing and how to handle unexpected genetic results.
The day before, ASCO dedicated an entire press conference for the more familiar treatments.
“New Approaches with Conventional Therapies” covered new uses of chemotherapies for ovarian and pancreatic cancers and results from a phase III trial comparing the breast cancer “biosimiliar” drug My1-1401O to trastuzumab, also known as Herceptin, one of the first targeted therapies developed and approved to treat HER-2 positive breast cancer.
The biosimiliar drug, a generic, cheaper version of trastuzumab, was equally as efficacious as trastuzumab, researchers from University of California, San Francisco showed. At 24 weeks, response rates were 69.6 percent with Myl-1401O and 64.0 percent with trastuzumab. It’s a “new milestone in the effort to bring cheaper versions of some of biotechnology’s best-known cancer drugs to the market,” a Wall Street Journal subhead read.
Valuing Cancer Care
This year, researchers from Rabin Medical Center in Israel added to that conversation, reporting that the price of cancer drugs in the U.S. is immensely higher than in other countries, and that treatments are still the least affordable in lower income countries. “If there are effective cancer therapies available in the West and not in developing countries, it will become a serious issue in coming years,” Daniel Goldstein, MD, of Rabin told STAT News.
In that same vein, the final plenary talk on value in oncology care was given by Deborah Schrag, MD, from the Dana-Farber Cancer Institute, a health services researcher focused on how to apply various value frameworks on the studies during the session. Her talk focused on the value of certain therapies, such as letrozole in the adjuvant setting and daratumumab for multiple myeloma. She also pointed out the average cost of chemo now is over $12,000 a month.
“Unaffordability of cancer prescriptions has adverse consequences,” one of Schrag’s slide read, which also called for “better policies to align care value with our core values.”
One doctor on Twitter called the talk “fabulous and provocative.” Schuchter agreed.
“Everyone in oncology should watch Deb Schrag’s #ASC016 plenary value discussion,” she tweeted on Monday. “Field changing.”