Doctors search for new ways to solve the puzzle of a rarebone cancer

Zach Sobiech (Image courtesy of YouTube)
Recently, the world watched as 18-year-old
Zach Sobiech transformed from ahigh school student living with cancer, to a rock star, living his dream ofrecording music and embracing his final days with friends and family. Zach losthis battle to a rare form of cancer on May 20, 2013, but his hit song “
Clouds” and story ofnever-ending hope, courage and conviction went viral and is now helping to raise awarenessabout a rare and devastating disease.
Osteosarcoma. It’s a million dollar word that many may neverknow. When we think about cancer, perhaps the words that come to mind mostimmediately are “lung,” “breast,” “prostate,” or “pancreas.” What we maynot think about is our bones.
Perhaps because our bones are hard and don’t change
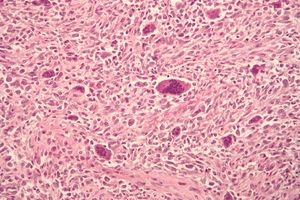
Osteosarcoma cells. (Image courtesy of Nephron, via Wikimedia Commons)
shape,many may not think of them as beingalive, but they are. Our bones are morethan just a part of our skeleton making up our arms and legs; they are livingtissue, comprised of living cells. These cells are responsible for controllingthe amount of minerals we store and forming the connective tissues that giveour bones strength. Like other parts of our bodies, the living cells in ourbones are also susceptible to cancer. Roughly 800 new cases of osteosarcoma –the most common type of bone cancer – are diagnosed each year. Nearly half ofthose new cases are found in children and teens.
Like Zach, who was diagnosed with cancer at age 14, mostosteosarcomas occur in children and young adults between the ages of 10 and 30.Though great advances have been made in the treatment of osteosarcoma over thelast several decades, national efforts are underway to learn more abouteffective treatment for the disease.
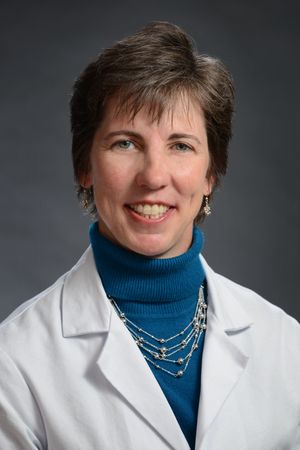
In this post, I sit down with Kristy L. Weber, MD, Penn Medicine’s new chief ofOrthopaedic Oncology and director of the Sarcoma Program at the Abramson Cancer Center,to learn about the latest advances in treating osteosarcoma and where researchfor this rare disease is headed.
 Q: Can you give us a brief overview of how far research and treatment of osteosarcoma has come in the last 50 years?
Q: Can you give us a brief overview of how far research and treatment of osteosarcoma has come in the last 50 years?
A: The long term view is that we’vecome a long way from the days when amputation was the primary method ofcontrol. Until the early 1970s,that was all we had, and even then, the survival rate was below 20percent. It wasn’t until specific chemotherapy agents came into play thatthe survival rates began to improve. Through the 1990s, chemotherapyregimens became more standardized, which contributed to the current 5-yearsurvival rate of 65-70 percent. In addition to multi-agent chemotherapy,sophisticated imaging techniques with modern MRI scans now allow orthopaediconcologists to accurately determine the extent of the tumor so they can betterplan surgical procedures. Finally, improvements in biomechanics,metallurgy, and engineering have allowed for the development of advanced prosthesesthat will provide patients who are candidates for limb salvage surgery with amore durable, longer-lasting reconstruction.
Q: Why is osteosarcoma so much more prevalent in children and teens?
A: During childhood and adolescence,the skeleton is in a rapid growth phase centered in the epiphyseal (growth)plates at the end of bones. These are the most common areas to findosteosarcomas. There are many biologic growth factors that have beenassociated with osteosarcoma and these are found in higher quantities whenpatients are in a growing phase.
Q: What are the biggest unanswered questions today?
A: The key piece of the puzzle we needto solve is how to prevent or treat spreading of the disease. We arepretty good at removing the local tumor in the bone, reconstructing theextremity, and maintaining relatively high function. However, there arestill too many patients whose tumors spread to other parts of the body(primarily the lungs) and die of their disease. Right now, most of theresearch in this area is focused on identifying target genes or signalingpathways that can be blocked to prevent tumor cells from spreading. Usinghuman cells grown in laboratories, we are able to test new drugs and learn moreabout potential treatment options. However, treating human patients isvery different from cell culture dishes, so results in the laboratory don’talways translate perfectly to the human situation.
Q: How can we improve the outcomes for patients with osteosarcoma?
A: I hope future research will help us gain a better scientificunderstanding of what happens that allows osteosarcoma to start in the firstplace. If we can identify where it starts, then we will be able to findways to prevent the progression of disease, or even prevent it from starting inthe first place. As with many cancers, we probably won’t find a single‘miracle drug.’ It will most likely take a cocktail of different drugs orbiologic agents to stop osteosarcoma.
Because this is a relatively rare disease, it isincredibly important that doctors across the country work together to test newtreatments. Clinical trials aimed at testing new treatment methodsrequire more patients than any one tumor center can find. The Children’sOncology Group (COG) is a collaborative effort that develops clinical trialsfor ostesosarcoma. The vast majority of children in the US withosteosarcoma are treated in a standardized way and often via clinical trials.At Penn and CHOP, we are focused on developing improved ways to treat patientswith this disease in addition to discovering novel ways to stop the cancercells from growing or spreading.
Q: What are the next surgical innovations for patients with osteosarcoma?
A: From a surgical standpoint, there are always twogoals: remove the tumor so that it never comes back, and give the patient thebest function possible after the reconstruction. In the last 20 years,metal prosthetic joints have become the most common method of reconstructionwhen an osteosarcoma is near a joint (knee, hip, shoulder). However,these prosthetics are made of metal and plastic parts, which will always wearout over time. The future of surgical reconstruction will hopefullyprovide more natural biologic solutions – such as ‘growing bones’ – that won’trequire multiple repeat surgeries.