When news broke last July ofthe American Society for Clinical Oncology’s
recommendation against PSA screeningin many groups of men,
Alan J. Wein, MD, professor and chief director, Division of Urology,
shared his insight for the PennMedicine News Blog. Wein noted thatthe test is worthwhile for some groups and not for others.
Now, almost a year later, new prostate cancer screening methods are garneringnational attention, and a Reuters article earlier this week discusses the cautious approach towards PSA testing taken by theAmerican College of Physicians. Arecent New York Times article suggests that these new tests can decrease the numberof “false alarms” from elevated PSA readings and prevent thousands of men fromreceiving unnecessary biopsies, surgeries, and radiation treatments. Some ofthe new tests look at the genetic workings of a cancer to identify dangeroustumors that need treatment, rather than slow-growing ones that may be best tomonitor only.
Considering these newdiscoveries, I checked in with David Lee, MD,FACS, assistant professor of Surgery in Urology, to see if any of these newtests influences the treatment he provides for patients.
News blog: What do you think of these new screenings that aregaining more attention now? Is the PSA test still a useful tool for somegroups?
Lee: The PSA is still extremely useful for all men. It is still the best blood test for screening for a particular type ofcancer. It is not a perfect test, but wholesale abandonment of PSAscreening will certainly result in many more men dying of prostatecancer. Because PSA can be elevated for a number of reasons, screeningfor prostate cancer as a whole can still be improved upon and new technologiesmay help us in this regard. I absolutely agree with the need for improvedscreening methods but all of these tests will likely never replace the PSA butbe used in conjunction with it.
News blog: Have you implemented any of these new tests in yourtreatment of prostate cancer patients?
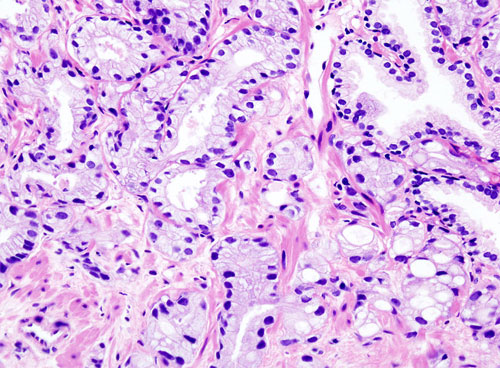
Lee: We have been using PCA3, a urine based assay,occasionally to help us screen some men who have a higher risk for prostatecancer based on a slightly elevated PSA and a biopsy that shows nocancer. This may help us decide when and if we need to offer anotherbiopsy at a future time for these men. There is a test called theProlaris test that we are in the process of implementing that can help todetermine whether a particular prostate cancer is more quickly growing thananother. This test uses RNA analysis of biopsied tissue to determineexpression of certain markers that are associated with cell division.
News blog: What’s the difference between watchful waiting andactive surveillance?
Lee: Watchful waiting is the process of diagnosingsomeone’s prostate cancer and then offering no active treatment or follow upuntil symptoms from spread appear. These men would then get treated withhormonal or chemotherapy agents. Active surveillance (AS) is the processby which urologists closely follow men with prostate cancer with serial PSA’s(usually every 3 months) and a periodic biopsy of the prostate (typically everyyear). However, the idea that active surveillance is more careful optionthan active treatment is quite dangerous. I think it is quite theopposite.
In some cases, a patient’soverall health suggests they are more likely to die of another cause beforetheir prostate cancer spreads. Alternatively, “if the patient has a long lifeexpectancy, say greater than 10 years, then even a very small and slow growingprostate cancer ought to be treated,” Lee adds.
News blog: So how accurate is the PSA test in regard to activesurveillance?
Lee: Methods for surveillance of someone with prostatecancer, consisting mainly of PSA and prostate biopsies, have been controversialdue to their less than optimal ability to detect prostate cancer. Whythen would someone undergoing active surveillance feel totally comfortablerelying on these tests then to determine when treatment is necessary? Atleast 30-40% of men that we perform radical prostatectomy on for Gleason 6 prostatecancer have a Gleason 7 at time of surgery. This reflects the inabilityof the prostate biopsy to adequately sample the prostate cancer so that weunderstand what type is really within the prostate. Additionally,prostate biopsy or PSA gives us no idea of how close to the edge of theprostate a particular cancer is growing. Therefore, a patient may have asmall cancer, but if it’s close to the edge, the cancer needs to grow only asmall distance before it is growing through the edge. When we findsomeone with an early prostate cancer, I think it is very reasonable to thinkthat this is fortunate opportunity to perform surgery because this is time thatsuch a treatment can cure someone permanently and if surveillance is performedthen we might miss that window. Therefore, even our surveillance methodsneed improvement. So, if someone is considering surveillance this must bethoughtfully discussed realizing the inadequacies that are present in thismethod of treatment.
Much like any othercondition, patients are encouraged to speak with their urologist on allavailable care options. “For the correctly selected patient, activesurveillance may be the best treatment,” Lee says.