As of September 2023, Penn Medicine’s official employee newsletter in print is Inside Penn Medicine. Many of our employee newsletter stories are now published throughout each month on the Penn Medicine News Blog. Older stories are available to browse in these archives.
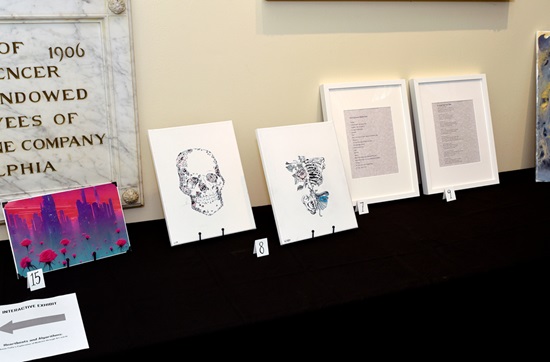
Pennsylvania Hospital’s Great Court recently became a hub for the arts, featuring colorful paintings, handcrafted textiles, and captivating photographs, all created by PAH staff and students.