“I’m sorry, but there’s nothing else we can do for you,” Ellen Bryant-Patterson recalls her former doctor telling her a few years ago. The 53-year old Philadelphian had just undergone a successful debridement to remove damaged tissue from her foot, but the doctor’s words shattered her hope.
Bryant-Patterson has Charcot foot, a complication of diabetes that causes the foot’s bones, joints, and tissues to weaken. Nerve damage limits sensation, and patients often develop wounds and infections; Bryant-Patterson struggled with a quarter-sized, non-healing ulcer that worsened every time she put pressure on her foot. But though Charcot foot is a progressive condition, it can be managed. As her doctor steered the conversation toward amputation and presented it as the only way forward, she knew it was time for a second opinion.
Her research brought her to the Wound Care Center at Penn Medicine University City (PMUC). The state-of-the-art center is the latest evolution of Penn Presbyterian Medical Center (PPMC)’s wound care program, which has been treating patients since 2007. In 2017, the center at PMUC expanded its footprint and its services, adding two hyperbaric oxygen chambers — and it continues to grow.
 “What started as a small clinic focused primarily on lower extremity wound care is now a multi-dimensional wound and hyperbaric medicine center dedicated to limb salvage. We cater to all wound types and customize treatment plans for faster healing,” said Ryan Dougherty, MBA, RN, assistant executive director of PMUC. “Our multidisciplinary team of seasoned wound-certified nurses and physicians in emergency medicine, vascular surgery, plastic surgery, dermatology, and podiatry works collaboratively to deliver optimal care to patients with the most complex wounds.”
“What started as a small clinic focused primarily on lower extremity wound care is now a multi-dimensional wound and hyperbaric medicine center dedicated to limb salvage. We cater to all wound types and customize treatment plans for faster healing,” said Ryan Dougherty, MBA, RN, assistant executive director of PMUC. “Our multidisciplinary team of seasoned wound-certified nurses and physicians in emergency medicine, vascular surgery, plastic surgery, dermatology, and podiatry works collaboratively to deliver optimal care to patients with the most complex wounds.”
Improving Outcomes with a Team-Based Approach
 The first faces patients see at the center are those of clinical coordinator Kelly Troiano, BSN, RN, MS, and her team of nurses, medical assistants, and patient services staff.
The first faces patients see at the center are those of clinical coordinator Kelly Troiano, BSN, RN, MS, and her team of nurses, medical assistants, and patient services staff.
Several of them worked together for years at the now-closed Graduate Hospital. In 2007, they moved as a group to the wound care clinic at PPMC, then again when the services transitioned to PMUC. The team’s extensive collective experience has proven hugely beneficial for both physicians and patients. Because patients are not always knowledgeable about their conditions, the team often needs to do some “detective work” to gather information about the wound and any other medical issues that may be affecting it.
“We’re a small, intimate group, and we’ve worked together for a long time,” she said. “Patients are assigned to a designated physician/nurse team. The patients become comfortable with this because it allows for continuity of care. It’s a really nice dynamic.”
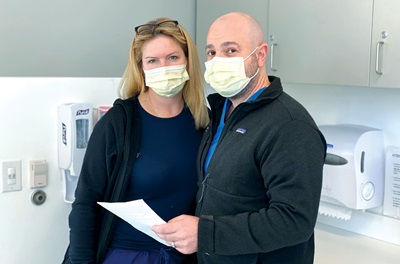
Kelly’s husband, Michael A. Troiano, DPM, a foot and ankle surgeon, took on Bryant-Patterson’s case in December 2019. “As soon as I came to Penn, I was on my way. Dr. Troiano did another debridement, then a reconstructive surgery on my foot. I took antibiotics for the infection, and I wore a boot to relieve pressure and help the wound close,” she said.
Troiano developed an interest in Charcot foot before he even entered medical school. However, he is the first to note that his surgical care is only “one small cog in a patient’s wheel.”
“For a patient like Ellen with a diabetic foot wound, you need an endocrinologist to ensure their A1C is appropriate. You need a nutritionist to ensure they have the albumin for healing. You need a vascular surgeon to ensure their blood flow is adequate. You need the prosthetist to make the brace so that when they heal, they can live happily ever after,” he said. “We have a comprehensive collaboration between experts who are the very best in their fields.”
Regardless of how many specialists are brought onto a case, they all share one goal: Saving the patient’s limbs.
“When someone loses a limb, there’s a 90 percent chance that they will lose a second limb within five years. And within five years of losing that second limb, there’s a 90 percent chance that they will die,” Troiano said. “By saving their limbs, they’re looking at another birthday, another opportunity to dance at a wedding, another chance to take a cruise. We take it very seriously, and our passion drives life-changing and life-saving care for our patients.”
Hyperbaric Medicine Takes Healing to the Next Level
 Following Bryant-Patterson’s surgeries, Troiano suggested hyperbaric oxygen (HBO) therapy to accelerate the healing process. Though she initially refused, citing claustrophobia, Troiano took her to meet the Hyperbaric Medicine technicians and get a better sense of what the therapy involved.
Following Bryant-Patterson’s surgeries, Troiano suggested hyperbaric oxygen (HBO) therapy to accelerate the healing process. Though she initially refused, citing claustrophobia, Troiano took her to meet the Hyperbaric Medicine technicians and get a better sense of what the therapy involved.
“There’s a lot of collaboration here because patients require numerous physician specialties to help them with their healing process,” said Mark Binkley, MD, medical director of Hyperbaric Medicine and an Emergency Medicine physician at PPMC. “When a physician has a patient that they think would benefit from HBO therapy, they consult us. We evaluate them and ensure there are no contraindications.” Patients who are eligible come in daily, Monday through Friday, for treatment.
When lying in an HBO chamber, patients breathe 100 percent oxygen at an elevated ambient pressure, which increases the amount of oxygen traveling through the bloodstream to damaged organs and tissue. Diabetic foot wounds are the most common conditions seen at the Wound Care Center, but HBO therapy can also be helpful for patients with compromised skin grafts or injuries caused by radiation therapy.
Encouraged by her family and care team, Bryant-Patterson ultimately underwent HBO therapy for 47 treatments. “The other doctor gave up on me, but Penn was trying to help, and it was time for me to help myself,” she said. “I was a nervous wreck, but it paid off. HBO was the key to my success.”
The quarter-sized ulcer that once threatened to claim her leg shrunk to the size of the dime, then fully healed. Bryant-Patterson regularly follows up at the center to treat her diabetes and monitor her Charcot foot condition, and she is diligent about keeping pressure off her foot. Though she can’t yet go without her trusty scooter, she is satisfied to take her recovery one day at a time.
“When I came to Penn, I was in bad shape. My foot was infected, I was frustrated and embarrassed by having to change my dressings twice a day for years, and I was depressed,” she said. “Dr. Troiano said, ‘I can’t make any promises, but I will do everything I can to get you through this.’ That was all I needed. Now, a year and a half later, I’m doing so much better. This experience has been a blessing, and I’m so grateful for him and for the staff at Penn.”