Gestational Diabetes Mellitus (GDM) is the most common type of diabetes diagnosed during pregnancy; it is also one of the most common pregnancy complications, affecting up to 18 percent of expecting women. Yet most women don’t learn much about the condition until after they are diagnosed.
GDM causes high blood sugar, which can negatively impact a woman’s pregnancy and the health of the baby. Women with GDM run the risk of delivering the baby preterm or having a baby with excessive birth weight or respiratory distress syndrome — a condition that makes breathing difficult. Babies of mothers with GDM may also experience low blood sugar (hypoglycemia) and have a higher chance of developing diabetes post pregnancy.
At 33 weeks into my pregnancy, I failed a glucose tolerance test and was diagnosed with GDM. Nothing really prepares you to hear a bad diagnosis. What can I say? I was upset and somewhat surprised. While I admit I hadn’t abstained from eating all “bad” foods during the pregnancy, my daily diet consisted largely of fruit, hearty salads, and home cooked meals for dinner. So how had I wound up with this awful diagnosis and what would come next for me and my baby?
My OB/GYN immediately scheduled me for a consultation with a dietitian. I almost broke down when I learned that I’d also have to head to the pharmacy to pick up a glucometer and that I’d be required to prick my finger four times a day to check my blood sugar levels and report my numbers to my doctor. That alone told me my life was about to change drastically… at least for the last two months of my pregnancy.
Goodbye Morning Fruit and Smoothies
Joan Metzner, RD, LDN, CDE, CLC, is a registered dietitian in the Helen O. Dickens Center for Women. Before our first meeting, Metzner asked me to keep a food diary for a few days. I was instructed to document the items in each of my meals. As she reviewed my diary entries, she circled every item that qualified as a carbohydrate that would eventually convert to sugar once in my system. Over half of the items I’d eaten that day were, in some form, sugar.
As a former marathon runner, I’ve always exercised a lot and therefore maintained a very free diet. I never counted carbs or calories because I figured whatever I ate would balance out with exercise. If you’ve never thought of your meals in terms of their contents (carbs vs fat vs protein vs fiber), hearing this explained for the first time is like learning a new language. Metzner helped me to understand that my pretzels, english muffin, rice and french fries all boiled down to the same thing: sugar. But that wasn’t the most surprising thing I learned. A big feature in my diet was fruit, which according to Metzner, was possibly one of the bigger culprits causing my blood sugar levels to spike.
“Consuming fruit in the morning is more of a concern for women with GDM because pregnancy hormones raise the blood sugar in the morning hours,” Metzner said. “Fruit is not recommended in the morning as it seems to increase blood sugars more so at this time of day.”
Metzner also advised consuming whole pieces of fruit instead of fruit smoothies.
“Solid food usually provides more satiety because the act of chewing and savoring food adds to the enjoyment of the meal and satisfies the appetite better, compared with simply swallowing a liquid. Solid food also takes longer to digest and keeps one full longer,” she said.
According to Metzner, it’s all about making sure every meal is balanced.
“Balanced meals are important for good health in general, but particularly for women with GDM who are relying on this as the primary strategy for blood sugar control,” she said. “Balanced meals, including lean proteins, whole grains and fruits, plenty of vegetables, and low fat sources of calcium are healthy choices for all.”
New research and making the GDM diet work
Metzner ended the session by telling me about a study that is currently underway at Penn. The “iPRO” study is led by Kimberly Trout, PhD, CNM, APRN, an assistant professor of Women’s Health at Penn’s School of Nursing, and Celeste Durnwald, MD, an assistant professor of Obstetrics and Gynecology and director of the Perinatal Diabetes Program at the Hospital of the University of Pennsylvania.
According to Trout, there have been very few studies about GDM diet recommendations. With funding from the Diabetes Research Center at Penn, Trout is working on establishing evidence-based guidelines for carbohydrates, protein, and fat consumption in patients with gestational diabetes.
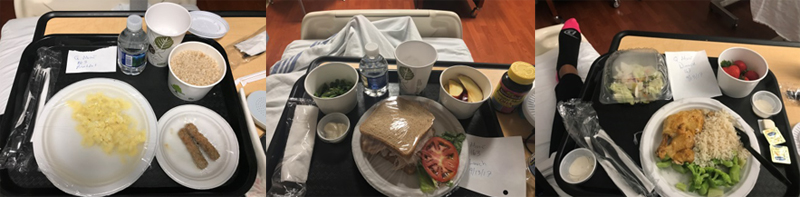
The study invites expecting mothers to spend four days and two nights in a hospital suite consuming meals prepared by a licensed dietitian while Trout and her team document the impact of varied protein consumption on controlling blood glucose.
I didn’t enroll in the study right away but I thought about it. After one week of seeing how difficult it was to purchase and prepare six to seven balanced meals/snacks per day, I decided participation in the study would be a much needed aid to my situation. I also reasoned that I’d get the opportunity to see some meal examples that would be good to replicate at home, and of course, my participation would contribute to helping women in the future to have an easier time managing their diets after receiving a GDM diagnosis.
I went into the study with no expectations but assumed they wouldn’t be rolling in any sweets or sodas for me to consume. I didn’t love every meal that was served but what I did love was hearing that my blood sugar numbers had remained at safe levels during my entire stay. And because I had a continuous glucose monitor installed, my pricked fingers got a much needed break.
In my opinion, one of the best perks of the study was that I didn’t have to prepare the meals. Cooking at home can be quite a hassle when you’re working full time, running a household, being a mother to an 8-year-old, and expecting a baby any day. One of the more difficult aspects of maintaining a healthy diet is finding time to prepare home-cooked meals, but a recent study, published in Public Health Nutrition, found that it certainly has its benefits.
Trout developed GDM when she was pregnant with her second child, and experienced firsthand how challenging it can be to suddenly have to follow a special diet during pregnancy. This ultimately fueled her interest in making GDM diets her primary area of research.
“I think it plays a huge role, especially for working moms,” Trout said. “It is so hard to find the time to do healthy meal preparation, but it is so essential.”
I must admit, I felt proud when on my next visit to the OB/GYN I’d lost seven pounds in my first two weeks on the diet.
Metzner says weight loss is not a goal of the GDM meal plan, but typically women lose a few pounds initially when they begin to avoid sweets and focus on portion control.
A week later my weigh-in was the same; I’d lost weight and the pounds had stayed off.
Next Steps
For reasons still unknown, GDM disproportionately affects non-Hispanic black, Hispanic, and American Indian/Alaska Native women, who are almost twice as likely to receive a diabetes diagnosis as non-Hispanic white adults. Half of all women with GDM will go on to develop type 2 diabetes, but with a proper diet and exercise, this can be avoided.
I look forward to getting back to my usual, active self once the baby is born and I definitely plan to be more mindful of my diet. I’m told that I’ll have to repeat the glucose tolerance test six weeks after giving birth and that my little one will be tested, too, to make sure I haven’t passed along the condition.
Trout’s study is still enrolling. She hopes to have results sometime next year and looks forward to translating the study’s findings into a diet program that could be made available to the community at large. Women interested in participating can contact her at ktrout@nursing.upenn.edu.