Care in the Community

The COVID-19 pandemic has disproportionately impacted communities of color, and particularly Black and Hispanic individuals. Combined with a summer of civil unrest sparked by police brutality, the pandemic has highlighted longstanding systemic inequities that have put the health of racial and ethnic minority groups at risk.
To break down barriers preventing underserved community members from accessing COVID-19 care, Penn Medicine leveraged its 16-year partnership with the Dr. Bernett L. Johnson Jr. Sayre Health Center. Adding to their list of collaborative clinical, research, educational, and advocacy initiatives, Penn and Sayre created a drive- and walk-through testing site in Cobbs Creek, a predominantly Black neighborhood in West Philadelphia. The site is one of nearly a dozen Penn Medicine COVID-19 testing sites serving communities throughout the region, including several testing sites that were stood up rapidly and efficiently in the earliest days of the pandemic.
In the first week alone, Sayre staff performed 906 tests. Since May, more than 15,800 Philadelphians have been tested there, and the site continues to run like a well-oiled machine, offering COVID-19 tests, behavioral health screenings, and flu vaccinations. The combination of barrier-free medical and behavioral health care ensures that people who have historically lacked access to resources feel seen and supported.
“Whether the result of the test is positive or negative, having access is an intervention in itself,” said Kent Bream, MD, Sayre medical director and an associate professor of Clinical Family Medicine and Community Health. “As people self-isolate, these kind of small but meaningful interpersonal interactions have been missing. Being here gives people a small sense that both we and they can control what’s happening.”
Drive- and walk-through COVID-19 testing is one of countless ways that Penn Medicine connects with underserved communities in need. Learn about the ways in which faculty, staff, and students have stepped up to support Penn Medicine’s neighbors through our new community impact report, Service in Action. Explore photos, animated graphics, videos, and more at CommunityImpact.PennMedicine.org.
In the Midst of a Struggle…

“History has shown that crises have a way of damaging our most vulnerable communities and COVID-19 is no different. Yet, when I came across this pin, I found some encouragement.”
In March, Claiborne B. Childs, MD, MS, director of Diversity & Inclusion Initiatives for the Internal Medicine residency program, rediscovered an inspiring lapel pin in his collection that he had purchased from the Smithsonian Museum of African American History last year. In a blog post for the Office of Inclusion and Diversity, Childs recalled the message that he took away from his experience at the museum: “Our ancestors showed us that in the midst of a struggle you don’t quit, you keep going.” The pin’s gold lettering not only offered him a timely reminder to remain resilient in the face of this newest struggle, the pandemic, but also a prescient message ahead of the civil unrest that spread a few months later.
Wise Words Within

Susan Summerton, MD, an associate professor of Radiology at the Perelman School of Medicine, usually reads mammograms and performs breast biopsies, but for a time, she shifted to chest imaging to help with the growing number of scans of patients with known or suspected COVID-19 infections. Summerton also took inspiration from the pandemic in her creative outlet—artwork she crafts from “letters” found in the human body in medical images—and delivered a crucial message in a blog post published by the Office of Inclusion and Diversity: “We should keep calm and stay home and soon we will all be on the other side of this dark time in our shared history.”
Celebrating Survivors

After three weeks at Chester County Hospital severely ill with COVID-19, Deborah Hocker was surprised with music, balloons, and a hospital lobby lined with staff cheering for her as she was discharged into her husband’s embrace. Hocker was the hospital’s first patient to be discharged after spending time on a ventilator. Penn Medicine’s other hospitals celebrated COVID success stories in a variety of ways, including playing “Here Comes the Sun” by the Beatles, and by planting a garden of colorful paper flowers outside HUP — one for each patient discharged.
Fighting an “Invisible Enemy”
In the early days of pandemic, many staff members across Penn Medicine were redeployed to new roles, some taking temperatures at hospital entrances, others communicating with patients via telemedicine. Taylor VanderWoude, RN, LT, a nurse in the Heart and Vascular ICU at the Hospital of the University of Pennsylvania, was also reassigned to help where she was needed most, though her mission took her out of the health system and into New York City.
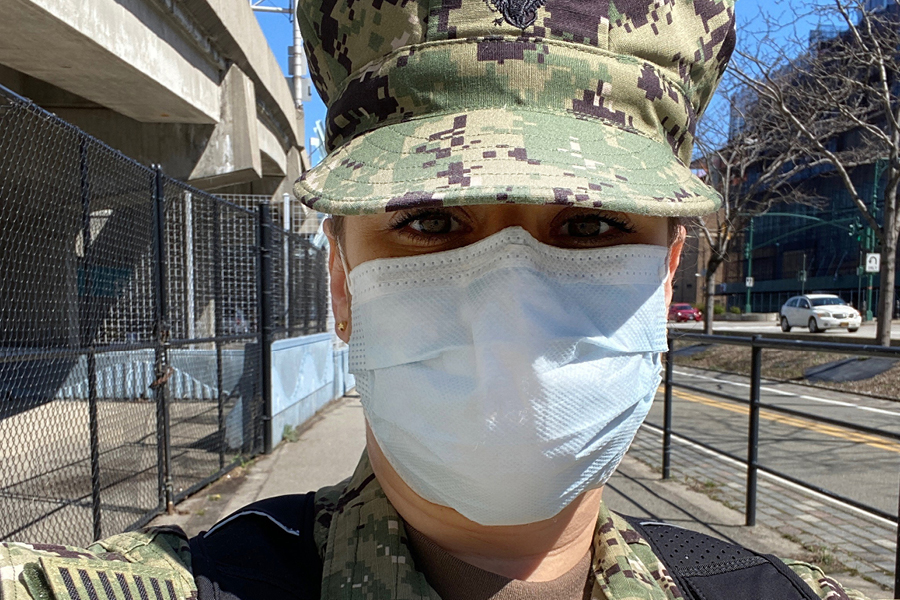
VanderWoude, a reservist in the United States Navy Reserve, was mobilized to the military-run medical center set up in the Javits Center, which treated more than 1,000 COVID-19 patients between its opening in March and closure in May. During those two “crazy” months, she often worked multiple shifts in a row and did her best to connect with patients in the ICU and provide their families with updates on their care. “We were working in a field hospital, so it was definitely different from our typical jobs. But we signed up to help people. You expect war, not a pandemic, but I was excited to help however I could,” she said.
Veterans Care Concierge liaison Paula Crawford-Gamble, CRNP, CAPT, NC, USN (Ret), could not have been more grateful for the “overwhelming support” that VanderWoude and nearly 20 other staff members received as their teams rallied around them. “Managers were calling me to make sure we could provide virtual farewell parties and mobilization packages. There truly was this recognition that whether you were in scrubs or a uniform, everyone was in this battle together.”
Kevin B. Mahoney, CEO of the University of Pennsylvania Health System, agreed. “I imagine this mobilization was different in many ways and not one that you trained for. It required you to make sacrifices, ones that not many would, to fight an invisible enemy on the home front,” he wrote in a letter thanking mobilized staff for their courage and commitment. “You continue to answer the call of those around you, whether in uniform or as civilians, and I’m honored to have you on board.”
Beginning a New Chapter in the COVID Era

“These extraordinary circumstances have brought out our best, and are making us an even stronger academic medical center. [...] The incredible work of our frontline providers during the surge of cases in the spring was beyond heroic. Their skill and compassion were enhanced by transformational changes in care delivery.”
In a letter welcoming the Perelman School of Medicine (PSOM) community back for another academic year, J. Larry Jameson, MD, PhD, dean of PSOM and executive vice president of the University of Pennsylvania for the Health System, offered a glimpse into the ongoing evolution of Penn’s campus, curriculum, and clinical research in response to COVID-19.
Health Care Heroes
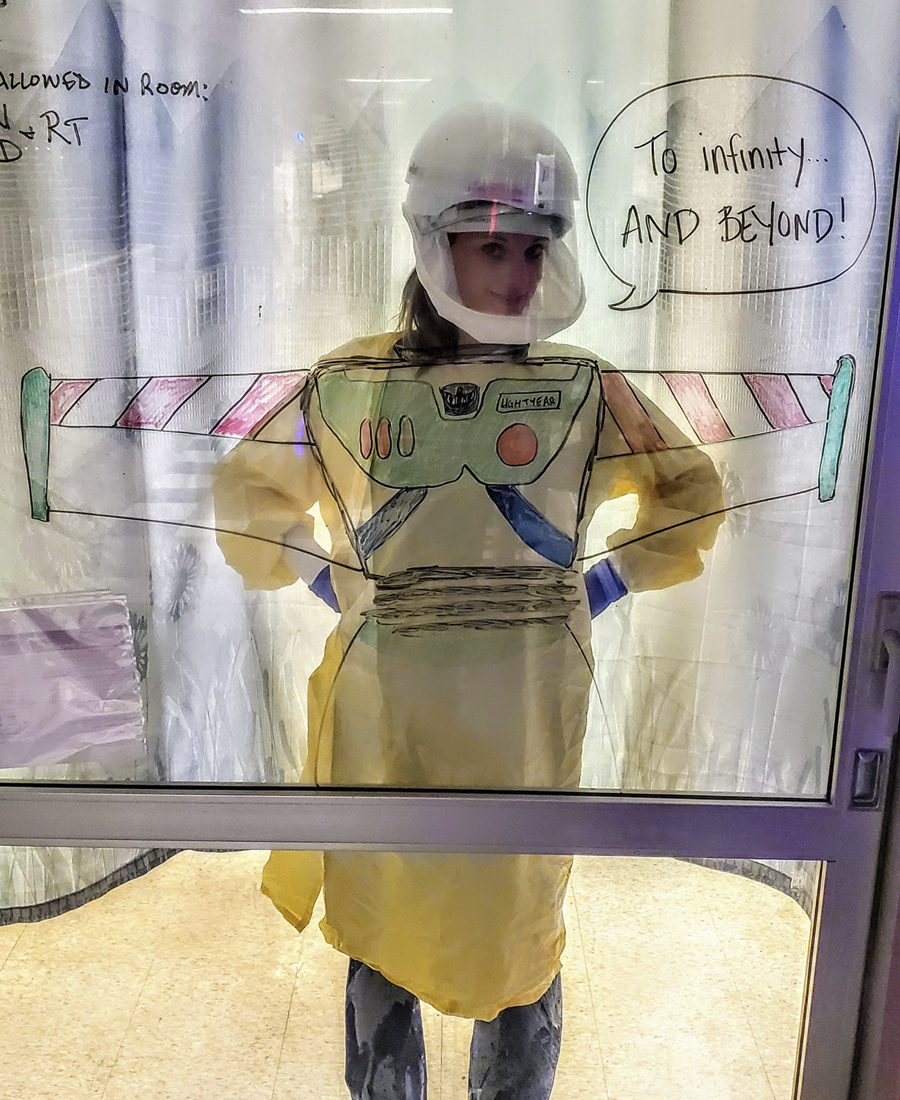
Katie Lord, BSN, RN, a nurse at the Hospital of the University of Pennsylvania, couldn’t “explain what coronavirus is or why mommy isn’t home” to her toddlers, but she could show them. While Lord stayed at a hotel between shifts this spring to avoid the potential to carry the coronavirus home, she and her colleagues drew inspiration from her personal protective equipment—and drew toy cartoon wings on the glass—to illustrate that she’s trying to be a hero just like her 3-year old’s idol, Buzz Lightyear.
Continuous Care

Life—and birth—goes on with or without a global pandemic. Across Penn Medicine, more than 11,300 babies have been born since early March. For the health system’s tiniest patients who need some extra time and support before they can head home with their families, staff like Rachelle Haworth, BSN, RN, a nurse in the Intensive Care Nursery at the Hospital of the University of Pennsylvania, are there to provide compassionate care they need.
More Lives to Save

“As our ICUs fill up with patients struggling to breathe, we look around and ask: Can we save a bed, can we save two beds, for the gunshot victims we know are coming next?”
In an impassioned piece for the New York Times, Elinore Kaufman, MD, MSHP, an assistant professor of Surgery in the Division of Traumatology, Surgical Critical Care, and Emergency Surgery, discussed the difficulties of balancing the global coronavirus pandemic with the nation’s gun violence epidemic and the consequences of both on desperately needed hospital resources.
Match Day 2020: Celebrating Amid Coronavirus

As Kate Hutchison and Scott Symonds sat on their couch with details of their futures in their hands, a range of emotions washed over them.
There was excitement to learn where they would go for residency after graduating from the Perelman School of Medicine (PSOM) in May. There was a tinge of disappointment, too; due to the COVID-19 pandemic and concerns about social distancing, the roommates were celebrating their long-awaited Match Day in their apartment rather than the atrium of the Jordan Medical Education Center. There was a sense of longing for their friends, families, and mentors, who, in normal times, would stand beside them cheering as they feverishly tore open their envelopes. But above all, they felt a wave of relief. In a world seemingly becoming more uncertain by the day, they finally had something concrete to hold onto. At noon, they would know where the next step of their medical training would take them.
“I’d been excited about residency for a long time, and it felt like everything going on in the world was overshadowing this milestone. But there are so many people who missed important events because of COVID. Even though this wasn’t exactly what we imagined, we were still in it together,” Symonds said of the home celebration in March.
To ensure their DIY Match Day was still special, Hutchison, Symonds, and his partner Ryan Kipp—a Penn State Hershey medical student who also matched this year—had flowers, cake, and champagne to celebrate, and their phones and laptops were charged and ready. In an effort to preserve some of the suspense, the friends wrote down each other’s matches and tucked them away in envelopes, even making one for Kipp’s dog, Mason.
One by one, they revealed their residency destinations: Back to the West Coast for Hutchison to train in orthopaedic surgery; and a pair of western Pennsylvania posts for Symonds and Kipp, at the University of Pittsburgh Medical Center for emergency medicine and Penn State Health in State College for family and community medicine, respectively. They immediately shared the exciting news with their loved ones, and their phones buzzed nonstop with updates from classmates.
“I probably got 20 times the amount of notifications I usually get in a day,” Hutchison said. “A lot of large-scale crises bring people together to support each other, but physical separation is required right now. It has been interesting to find different ways to build community and togetherness. There has been a lot of FaceTiming!”
Of the 155 PSOM students who matched this March, 30 percent stayed at Penn, joining residency programs at the Hospital of the University of Pennsylvania, Pennsylvania Hospital, Scheie Eye Institute, and CHOP, while the other 70 percent scattered across 27 different states—all facing an unprecedented challenge of beginning residency amid a global pandemic.
“I know that this is not the format for Match Day that we all planned for, but I hope that you find joy in your accomplishments,” said Suzanne Rose, MD, MSEd, senior vice dean for Medical Education at PSOM. “You all have the determination, creativity, resilience, and compassion to rise to the current challenges and to face your very bright futures.”
Facing the Uncertainty
When a group of first-year medical students joined together with the goal of creating a literary magazine fused with scientific communication, they never expected that “a pandemic would leap out of our lecture slides and into our reality.” But even as they spread across the country to self-isolate, their creative venture, apenndx, did not fall by the wayside. Rather, another wave of submissions flooded in, offering snapshots of students’ COVID-19 experiences. The excerpts below represent a selection of those perspectives.
“Learning how to listen, to empathize, to do reflection, to dwell with ambiguity…. These are also critical physician skills, and the arts and humanities help to promote that,” said Horace DeLisser, MD, associate dean for Diversity and Inclusion, in an interview with the Philadelphia Inquirer.
My Heart Aches, But
To connect with the memory of her mother—a surgeon, poet, and avid runner—fourth-year Perelman School of Medicine student E. Berryhill McCarty has hit the pavement, running at least one mile and writing a haiku to accompany a photo snapped every day. Through her three-line verses, some of which reflect on the bright spots of normalcy that remain in “a world so changed,” others revealing her uneasiness in this “grim” new era, McCarty has been able to process her feelings throughout the pandemic. A collection of her poems and photos was published in the inaugural issue of apenndx.
Philly’s Children Are Our Children
“As many of us gradually exit quarantine with celebration, our city’s children will need even more resources for the additional challenges they will face during this chronic readjustment phase.”
In a city where health, food security, graduation rates, and more are largely determined by zip code, the socioeconomic impact of COVID-19 will linger long after businesses and schools reopen. First-year MD-PhD students Likhitha Kolla and Diane Rafizadeh discussed the resources Philadelphia’s most vulnerable children need to cope with this ever-changing new normal in an apenndx essay.
Find apenndx online at http://www.apenndx.com.
ICYMI: In COVID You Missed It
COVID-19 has dominated the headlines, but even during a pandemic, new Penn Medicine research findings from a range of disciplines found their way to publication in top journals. In case you missed it, here are some highlights.

By the time a patient is diagnosed with pancreatic cancer, the disease has most likely spread; it’s one of the deadliest cancers. Catching it early is vital in order to connect patients with treatment. A Penn team recently found that a liquid biopsy can detect the most common form of pancreatic cancer in its early stages by screening for multiple biomarkers. The test was more accurate at detecting disease in a blinded study than any other known biomarker alone, and was also more accurate at staging disease than imaging is capable of alone, according to the study published in Clinical Cancer Research. This finding was one of several significant steps forward for liquid biopsy approaches for cancer this year. Another Penn team found that imaging of glioblastoma—another of the deadliest cancers—can determine whether a more-invasive surgical biopsy is needed. Others showed a liquid biopsy could identify patients with metastatic non-small cell lung cancer most likely to benefit from immunotherapy treatment.

In a study published in JAMA Network Open, Penn researchers found that between 2005 and 2016, doctor’s office visits for ongoing muscle relaxant prescriptions tripled nationally from 8.5 million to 24.7 million, largely among older adults. Nearly 70 percent of these patients also received prescriptions for opioids. The team hypothesized that the spike in muscle relaxant prescriptions was a response to the opioid epidemic, but noted that they can have potentially adverse effects—especially when combined with opioids—and may not be more effective than Tylenol or Advil. The findings suggest further research is needed to understand the effects of long-term use of muscle relaxants, and that patients need access to better options for pain management.

Millions of babies have been born with the aid of assisted reproductive technology (ART), but some moms can experience complications. Penn researchers conducted a study in mice to explore the underlying cause of placental abnormalities, preeclampsia, and abnormal fetal growth. They examined how four steps of the ART process impacted placental development and fetal growth. The mouse models indicated that the embryo culture—where the fertilization of the egg with the sperm takes place in a medium meant to replicate the oviduct’s essential nutrients and is placed in an incubator that mimics the womb—had the strongest effect on adverse outcomes, and the abnormalities were unrelated to infertility. The findings, which were published in Development, suggest that optimizing the embryo culture process may ensure healthier outcomes.

Penn Medicine Ranked Among Top Hospitals in the Nation
Penn Medicine hospitals have once again been ranked among the top hospitals in the nation by U.S News & World Report. Out of more than 4,500 hospitals analyzed nationwide, Penn Medicine is among only 20 institutions to be named to this year’s Honor Roll, and the only one in the Philadelphia region.
The combined enterprise of the Hospital of the University of Pennsylvania and Penn Presbyterian Medical Center was recognized for the 14th consecutive year, earning distinction as the #1 hospital in Pennsylvania and in the Philadelphia metro area. HUP-PPMC also received top marks among 12 clinical specialties and in all 10 of the common adult procedures and conditions evaluated by the survey.
Lancaster General Health ranked #4 in the state, and was nationally ranked in Orthopedics. Pennsylvania Hospital was named #4 in Philadelphia, #8 in the state, and was nationally recognized in Gynecology. Chester County Hospital earned #5 in the Philadelphia region, #10 in the state, and national distinction in Diabetes & Endocrinology. Princeton Health ranked #9 in New Jersey, #24 in the New York metro area, and was recognized as high-performing in Orthopedics.
PSOM Named Top Training Ground

The nation’s first medical school continues to rank among the best in the United States, according to U.S. News & World Report’s annual “Best Graduate Schools” report.
For the second consecutive year, the Perelman School of Medicine (PSOM) was ranked #3, continuing a 23-year streak among the top-ten research-oriented medical schools. PSOM, which is also consistently among the nation’s top recipients of federal funding from the National Institutes of Health, earned additional top marks in eight areas of specialty training: Pediatrics, Internal Medicine, Obstetrics & Gynecology, Radiology, Anesthesiology, Psychiatry, Surgery, and Family Medicine.
“The Perelman School of Medicine has an international reputation for unique training programs and a groundbreaking curriculum which combines basic sciences and clinical experience, preparing students for a future of innovative research and patient-centered care,” said J. Larry Jameson, MD, PhD, dean of PSOM and executive vice president of the University of Pennsylvania for the health system. “This continued recognition exemplifies Penn’s rich tradition of scientific discovery and academic excellence. We are so proud of the incredible learning environment in our clinics and labs, our inspiring faculty, and our inquisitive students.”
Roberts Proton Therapy Center Celebrates 10 Years of Achievements

In January 2010, the first patients received treatment at the newly opened Roberts Proton Therapy Center. Featuring a technology that was revolutionary at the time, Penn Medicine brought scientific rigor to a new radiation therapy modality in a facility that remains the largest, most comprehensive proton therapy center of its kind.
Perhaps the center’s most important research contribution to the field of proton therapy was a study published in JAMA Oncology in December 2019 that evaluated patients with non-metastatic brain, head and neck, lung, gastrointestinal, and gynecologic cancers. The research delivered scientific proof of its ability to significantly lower the risk of side effects while having almost identical cure rates to traditional radiotherapy. “Even we did not expect the effect to be this sizeable,” said senior author and Radiation Oncology Chair James Metz, MD.
Mourning a Beloved Benefactor: Suzanne Roberts

Any celebrations of these accomplishments would have been bittersweet because of the passing of Suzanne Roberts in April 2020. Known as a woman of many talents—as an actress, broadcaster, and educator—she was devoted to having a positive impact on the world, which made her a proud contributor to her family’s landmark gift creating the Roberts Proton Therapy Center. She and her late husband, Ralph, never missed the center’s annual Proton Patient Alumni reception, and guests looked forward to and were inspired by her presence. Perelman School of Medicine Dean J. Larry Jameson shared, “Suzanne’s boundless compassion and energy will surely be missed at Penn Medicine and in the greater Philadelphia community. Her vibrant positivity was a treasure for our patients and physicians.”
Howell Takes the Helm as OB/GYN Chair

Elizabeth Howell, MD, MPP, has been named chair of the Department of Obstetrics and Gynecology in the Perelman School of Medicine (PSOM) at the University of Pennsylvania. She joined Penn in September after more than 20 years at the Icahn School of Medicine at Mount Sinai, where she most recently served as the director of the Blavatnik Family Women’s Health Research Institute and a professor of Obstetrics, Gynecology, and Reproductive Science, Psychiatry, and Population Health Science and Policy.
Howell has served on several expert committees, scientific advisory boards, and editorial boards, published a wealth of policy-shaping research in premier academic medical journals. Her work primarily focuses on the impact of racial and ethnic disparities on maternal and infant health and mortality.
Howell succeeds Deborah Driscoll, MD, who in 2019 was named vice dean for professional services of PSOM and senior vice president of the Clinical Practices of the University of Pennsylvania. Driscoll’s 14 years of transformative leadership propelled innovative work in areas ranging from pregnancy loss to remote monitoring for new mothers and led Penn Medicine’s OB/GYN department to become a renowned leader in research, clinical care, and education.
Sensory Processing Expert Begins as Neurosurgery Chair

Daniel Yoshor, MD, was appointed chair of the Department of Neurosurgery for the Perelman School of Medicine (PSOM) and vice president of clinical integration and innovation for the health system in July. A dynamic leader and accomplished administrator, he held several appointments in Neurosurgery, Neurology, and Neuroscience over the past 20 years at Baylor College of Medicine in Houston, most recently serving as the Marc J. Shapiro endowed professor and chair of Neurosurgery.
Yoshor’s research centers on the mechanisms of sensory processing in the visual cortex. His team has learned to bypass the optic nerve and send visual information straight to the brain, which helps blind people to “see” shapes. He also has extensive experience in endoscopic pituitary and skull base surgery, brain tumor and epilepsy surgery, clinical brain mapping, and developing neuro-technologies.
His appointment comes after longtime chair M. Sean Grady, MD, transitioned to the role of physician director of the Neurosciences Service Line. Grady’s exceptional, energetic leadership led to advanced research in areas like traumatic brain injury, a substantial increase in the amount of female residents, and the development of patient-centered programs like the Mind Your Brain Conference.