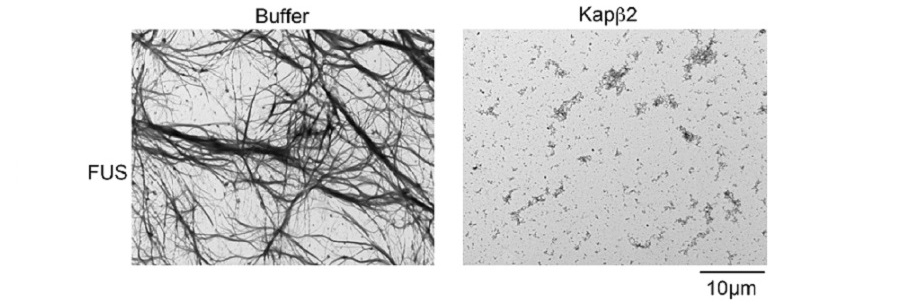
Dense FUS protein fibrils form in the absence of nuclear-import receptors (NIRs, left), but are disrupted when NIRs are present (right).
James Shorter, Perelman School of Medicine, University of Pennsylvania; Cell
PHILADELPHIA – A host of special molecules called nuclear RNA-binding proteins (RBPs), when misplaced outside the nucleus, form the harmful clumps seen in several brain disorders, including frontotemporal dementia (FTD) and amyotrophic lateral sclerosis (ALS). “Clumps that form from these disease proteins are composed of sticky fibrils that damage nerve cells,” said James Shorter, PhD, an associate professor of Biochemistry and Biophysics in the Perelman School of Medicine at the University of Pennsylvania. “We want to reverse the formation of these clumps and put the RNA-binding proteins back in their proper place, inside the nucleus.”
Normally, nuclear-import receptors (NIRs) bind to specific sequences of amino acids on the RBPs, to shepherd them into the nucleus. A team led by Shorter, describes in Cell this week what happened when they added NIRs to aggregates made from TDP-43 and FUS proteins, which are connected to these neurodegenerative diseases.
“When we increased the concentration of NIRs, there were three important and surprising outcomes,” said co-first author Lin Guo, PhD, a Target ALS Springboard Fellow. First, clumps of RBPs dissolved in test-tube experiments. Next, NIRs also dissolved cytoplasmic clumps in cells and functional RBPs were returned to the nucleus. And finally, when the expression of NIRs was increased in fruitfly models of disease, lifespan was extended and degeneration was reduced.
“All of this biochemistry was highly unanticipated,” said co-first author Henry Wang, an MD/PhD student at Penn. “We didn’t suspect that the NIRs would break up the clumps, return the RBPs to the nucleus, and mitigate neurodegeneration.”
The team was surprised by how rapidly the NIRs could reverse the formation of the FUS and TDP-43 clumps. The transition from the RBP being dissolved in solution to forming droplet-like structures normally happens in the nucleus as a regular part of RBP function. However, when RBPs, like FUS and TDP-43, are misplaced in the cytoplasm, these phase changes can become aberrant, setting the RBPs on a destructive path, which can be corrected with NIRs. But, NIR expression or activity likely becomes reduced in disease.
‘Given this complexity, we are now working to find a way to increase expression or activity of NIRs in neurons with clumps using protein engineering or small-molecule drugs, said coauthor Charlotte Fare, a doctoral student in Shorter’s lab.
Collaborators include co-senior author J. Paul Taylor, MD, PhD, an investigator with the Howard Hughes Medical Institute and chair of Cell and Molecular Biology at St. Jude Children’s Research Hospital; Clotilde Lagier-Tourenne, Mass General Hospital; Yuh Min Chook, University of Texas; and Udai Pandey, University of Pittsburgh.
This research was funded by the National Institute of Health (R21NS090205), Target ALS, the ALS Association, and the The Robert Packard Center for ALS Research at Johns Hopkins.
http://www.cell.com/cell/fulltext/S0092-8674(18)30282-4
Penn Medicine is one of the world’s leading academic medical centers, dedicated to the related missions of medical education, biomedical research, excellence in patient care, and community service. The organization consists of the University of Pennsylvania Health System and Penn’s Raymond and Ruth Perelman School of Medicine, founded in 1765 as the nation’s first medical school.
The Perelman School of Medicine is consistently among the nation's top recipients of funding from the National Institutes of Health, with $550 million awarded in the 2022 fiscal year. Home to a proud history of “firsts” in medicine, Penn Medicine teams have pioneered discoveries and innovations that have shaped modern medicine, including recent breakthroughs such as CAR T cell therapy for cancer and the mRNA technology used in COVID-19 vaccines.
The University of Pennsylvania Health System’s patient care facilities stretch from the Susquehanna River in Pennsylvania to the New Jersey shore. These include the Hospital of the University of Pennsylvania, Penn Presbyterian Medical Center, Chester County Hospital, Lancaster General Health, Penn Medicine Princeton Health, and Pennsylvania Hospital—the nation’s first hospital, founded in 1751. Additional facilities and enterprises include Good Shepherd Penn Partners, Penn Medicine at Home, Lancaster Behavioral Health Hospital, and Princeton House Behavioral Health, among others.
Penn Medicine is an $11.1 billion enterprise powered by more than 49,000 talented faculty and staff.