Diabetes Diet Instruction
It is important to maintain optimal blood glucose when you have diabetes to avoid complications that can impact your overall health. The diet you should follow contains a controlled intake of carbohydrates which is balanced with adequate amounts of protein and other food groups. Consuming too many calories can cause your blood glucose to elevate.
 While these instructions sounded very clear to the nurse who wrote them, that wasn’t the case for her patient, who had just been diagnosed with diabetes in the hospital. He didn’t understand and was afraid to ask questions. A week after being discharged, he returned to his doctor’s office with blood sugar that was sky high.
While these instructions sounded very clear to the nurse who wrote them, that wasn’t the case for her patient, who had just been diagnosed with diabetes in the hospital. He didn’t understand and was afraid to ask questions. A week after being discharged, he returned to his doctor’s office with blood sugar that was sky high.
Although this case is hypothetical, it represents a serious concern in today’s health-care environment: health illiteracy or the inability to understand basic medical information. This gap in understanding is not only leading to increased readmissions but also increased mortality. “We need to change how staff teach so patients can learn to care for themselves,” said Carolyn Cutilli, PhD, RN, Patient Education specialist at the Hospital of the University of Pennsylvania. And that’s precisely what Cutilli and HUP’s other patient education specialists do: They work with staff to ensure that patients fully understand what’s important to stay healthy.
First, keep it simple. “Where’s the beef?” – Wendy’s catchphrase from 30 years ago – still resonates with people. It’s stuck with us. And that’s the way patient education needs to be: it must stick with both patients and families. “We need to talk with patients to learn what will get their attention and motivate them to make changes," Cutilli said. For example, a patient who’s having trouble maintaining a low-salt diet (and has been readmitted more than once for congestive heart failure) tells her nurse that more than anything she wants to go to her granddaughter’s wedding. “To make this happen she needs to stay healthy.... Now you’ve got motivation.”
In the hospital setting, patient education material like pamphlets or instruction sheets not only provides consistent and evidence-based information but also serves as a tool patients can refer to after discharge. So the information has to be clear and concise. Maureen Bonnell, BSN, RN, Patient Education specialist, worked with staff of HUP’s postpartum unit to develop a pamphlet on Neonatal Abstinence Syndrome, a medical condition brought on by women who take opiates while pregnant, which often results in the baby experiencing withdrawal symptoms after birth. In reviewing the draft of the brochure, she checked to make sure the information used simple words and was patient friendly, with the right readability. And she made sure there was patient input in developing the pamphlet. “Patients have to be involved from the start… especially if it’s an uncomfortable topic to discuss,” Bonnell said.
Clinicians often lapse into medical jargon when talking to patients and families, which can lead to dangerous results. Indeed, studies show that up to 80 percent of the medical information patients hear from a clinician is quickly forgotten, and nearly half of what's remembered is incorrect. This is where teach-back comes in, a method of confirming that a patient truly
understands what is being explained. As the term implies, it ensures that the patient can “teach back” – and not just recite from memory -- the information he or she heard from a clinician.
Teach-back has three basic goals: making sure patients have the basic knowledge (ie, the patient knows he has to take a pill), the right attitude (he understands why), and the desired 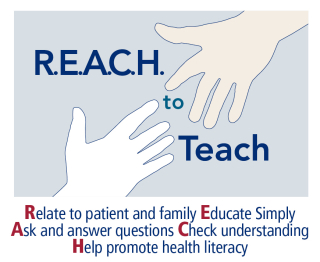 behavior (he knows he has to take with food). But teach-back is not a test of the patient's knowledge. Rather it is a test of how well clinicians explained the concept.
behavior (he knows he has to take with food). But teach-back is not a test of the patient's knowledge. Rather it is a test of how well clinicians explained the concept.
To help make the health literacy message “stick” with staff, patient and family education leaders from throughout the Health System created the R.E.A.C.H to Teach graphic which highlights the most effective way to educate patient and families. Cutilli recently published the article “R.E.A.C.H. to Teach: Making Patient and Family Education ‘Stick’” in Orthopaedic Nursing describing the use of these marketing concepts for patient education.
Oh and in case you’re wondering, below is the revised – and much more effective - version to explain proper nutrition to patients.
What to eat when you have diabetes:
- Eating right helps your blood sugar.
- You can eat many of the same foods you already eat.
- Eat smaller amounts (portions) of food.
- Eat fewer carbohydrates. Examples include sweets (cookies, candy), breads, potatoes, cereals, rice, sodas, juices, and fruit.
- Eat proteins every day. Examples of protein are chicken, steak, fish, eggs and tofu.
- Vegetables like broccoli, spinach, and green beans are good for your diet. You can usually eat as many as you want.
Photo caption: Patient Education specialist Maureen Bonnell (r) reviews a patient education pamphlet with Kate Elliott of HUP's postpartum unit.