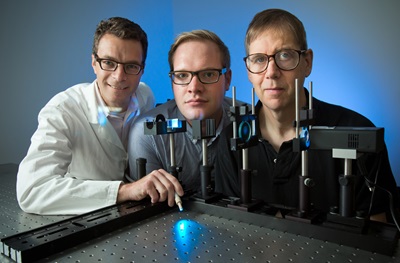
Photo credit: Tommy Leonardi
PHILADELPHIA
– The eyes are for seeing, but they have other important biological functions, including automatic visual reflexes that go on without awareness. The reflexive system of the human eye also produces a conscious, visual experience, according to a new study from researchers in the Perelman School of Medicine and School of Arts and Sciences at the University of Pennsylvania. The findings, reported today in the
Proceedings of the National Academy of Sciences, may provide insight into the excessive light sensitivity sometimes experienced by people with eye disease, migraine headaches and concussions.
The study addressed the properties of melanopsin, a blue-light sensitive protein in the eye that establishes the rhythm of the day-night cycle and the familiar constriction of the pupil to bright light. The researchers created a special pulse of light that stimulates only the melanopsin cells of the eye. They showed this light pulse to people and measured their pupil response and brain activity, as well as asked them what they saw. Remarkably, they found that people have brain activity and a visual experience in response to a light that is invisible to the parts of the eye normally used for seeing.
“Melanopsin is a part of our visual system from long ago in evolution, and it controls several important biological responses to light," said lead author, Manuel Spitschan, PhD, who received his doctorate from the Psychology program at Penn in 2016 and is now a Sir Henry Wellcome Postdoctoral Fellow at the University of Oxford. “It has been hard to know if we have a visual experience that accompanies these reflexes, as any normal light that stimulates melanopsin will also stimulate the cone cells of the eye that support our regular vision. We wouldn't know whether what a person sees arises from melanopsin or the cones.”
To solve this problem, the Penn team developed a special kind of light pulse that stimulates melanopsin but is invisible to the cones. The lights were created using a machine that can sculpt and switch between computer-designed “rainbows” of light. First, the researchers had people watch these light pulses while their pupil response was recorded. The scientists confirmed that a light pulse that is invisible to the cones evokes a slow, reflexive constriction of the pupil that is characteristic of melanopsin stimulation. They then measured brain activity using the technique of functional MRI, and found that the visual pathway of the brain responds to the melanopsin stimulus.
“This was a particularly exciting finding,” said senior author Geoffrey K. Aguirre, MD, PhD, a behavioral neurologist and an associate professor of Neurology at Penn. “A neural response within the occipital cortex strongly suggests that people have a conscious experience of melanopsin stimulation that is explicitly visual.”
The researchers then asked what people “see” with melanopsin. They had 20 people look at the pulses of light and provide ratings of different perceptual qualities. People described the melanopsin stimulus as a blurry kind of brightness, in contrast to the focused experience provided by the cones. They also described the melanopsin light pulse as unpleasant.
“This perceptual experience fits with what we know about the cells that contain melanopsin,” said David H. Brainard, PhD, the RRL professor of Psychology. “There are relatively few of these melanopsin cells in the eye. Like a digital camera that doesn't have many pixels, we would expect the melanopsin system to give a blurry, indistinct image of the world.”
Their work has particular relevance for understanding the experience of people with photophobia, who are overly sensitive to bright light and experience pain as a result. “Research in mice makes us think that melanopsin contributes to the sensation of discomfort from very bright light,” Aguirre said. “Subjects in our study found the melanopsin stimulus to be unpleasant, and people with photophobia may experience a stronger form of this response to melanopsin. We now have a tool to help us to better understand excessive light sensitivity.”
This work was supported by National Institute of Health grants (R01 EY024681, P30 EY001583, and NS045839), and a Department of Defense grant (W81XWH-15-1-0447).
Editor’s Note: A patent on the technique of selectively and robustly stimulating the light-sensitive cells of the eye and its applications has been filed by the University of Pennsylvania with Aguirre, Brainard, and Spitschan as inventors.
Penn Medicine is one of the world’s leading academic medical centers, dedicated to the related missions of medical education, biomedical research, excellence in patient care, and community service. The organization consists of the University of Pennsylvania Health System and Penn’s Raymond and Ruth Perelman School of Medicine, founded in 1765 as the nation’s first medical school.
The Perelman School of Medicine is consistently among the nation's top recipients of funding from the National Institutes of Health, with $550 million awarded in the 2022 fiscal year. Home to a proud history of “firsts” in medicine, Penn Medicine teams have pioneered discoveries and innovations that have shaped modern medicine, including recent breakthroughs such as CAR T cell therapy for cancer and the mRNA technology used in COVID-19 vaccines.
The University of Pennsylvania Health System’s patient care facilities stretch from the Susquehanna River in Pennsylvania to the New Jersey shore. These include the Hospital of the University of Pennsylvania, Penn Presbyterian Medical Center, Chester County Hospital, Lancaster General Health, Penn Medicine Princeton Health, and Pennsylvania Hospital—the nation’s first hospital, founded in 1751. Additional facilities and enterprises include Good Shepherd Penn Partners, Penn Medicine at Home, Lancaster Behavioral Health Hospital, and Princeton House Behavioral Health, among others.
Penn Medicine is an $11.1 billion enterprise powered by more than 49,000 talented faculty and staff.