| > |
Researchers at the University
of Pennsylvania School of Medicine have identified
proteins in the rod and cones of the eye that could lead
to the discovery of the genetic causes of a host of inherited
eye diseases. |
| > |
The researchers used mass spectrometry
to identify and measure the amounts of proteins in mouse
photoreceptor sensory cilia, the light-sensing parts of the
eye’s retina. They found many proteins in
the cilia that had not been identified in photoreceptors
before.. |
| > |
The investigators also found 60 proteins
encoded by genes on chromosomes implicated in 23 inherited
cilia-related disorders. Armed with this knowledge, researchers
hope to be able to more quickly find the exact genetic mutations
that cause these 23 cilia diseases, which include eye and
kidney diseases, among others. |
| > |
The study will appear in the August print
issue of Molecular & Cellular Proteomics and
has been pre-published online. |
(PHILADELPHIA) – Researchers at the University
of Pennsylvania School of Medicine have identified proteins in the rod and cones of the eye that could lead to the discovery of the genetic causes
of a host of inherited eye
diseases. The investigators hope
to gain a clearer understanding of what goes wrong at the most
basic level in these diseases that cause blindness and other disorders.
 |
|
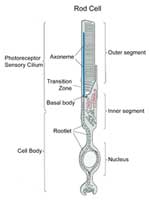
Photoreceptor sensory cilia (top part of rod cell) are the light sensitive parts of the rods and cones in the eye's retina.
Click on thumbnail
to view full-size images
|
Specifically, they have identified and measured the types and
amounts of proteins in the light-sensing parts of the eye’s
retina. These light-sensitive structures, called photoreceptor sensory cilia, enable the rod and cone cells of the retina to detect
light. While the proteins of cilia in single-celled organisms have
been studied, this is the first time that a comprehensive description
of the proteins of a mammalian cilium – used for movement
and sensing – has been determined.
“We want to understand how cilia work normally and how their
function is disrupted in disease, because their dysfunction is
such an important cause of disease,” says senior author Eric
A. Pierce, MD, PhD, Associate Professor of Ophthalmology at the
F.M.
Kirby Center for Molecular Ophthalmology at Penn. “One
of the first steps to achieve this is to put together a complete
parts list. Now that we have that, we can figure out how all 2000
proteins we’ve identified fit together correctly.”
The study will appear in the August print issue of Molecular & Cellular
Proteomics and has been pre-published online.
 |
|
Isolated mouse photoreceptor sensory cilium. The rootlet is in red and the axoneme in green.
Click on thumbnail
to view full-size images
|
Cilia, specialized structures that extend from cells, have recently
taken the spotlight in studying genetic diseases. They are commonly
used by cells for movement or sensory purposes, and, in many cases
with mammals, have been thought to be remnants of evolution without
much purpose. But new research has shown that mutations in genes that encode the proteins of cilia are common causes of a host of
genetic diseases, including inherited retinal
diseases and polycystic
kidney disease.
Cilia diseases can also affect multiple organ systems in such
disorders as Bardet-Biedl
Syndrome, which causes kidney
disease,
obesity, polydactyly, diabetes, and retinal degeneration; Senior-Loken
Syndrome, which causes kidney disease and retinal degeneration;
Joubert
Syndrome, which causes neurological disease, kidney disease,
and retinal degeneration; Usher
Syndrome, which causes deafness and blindness; and Meckel
Syndrome, which causes kidney disease
and neural
tube defects.
Lead author Qin
Liu, MD, PhD, Research Assistant Professor, and
Pierce collaborated with a team at The
Wistar Institute led by
David
Speicher to perform the analyses for this study. The
researchers used mass
spectrometry to identify and measure the
amounts of proteins in mouse photoreceptor sensory cilia. They
found many proteins in the cilia that had not been identified in
photoreceptors before. This includes proteins involved in intraflagellar
transport, which is a process that moves materials from the cell
body into the cilia. Mutations in proteins associated with this
transport system lead to a number of cilia-related diseases.
The investigators also found 60 proteins encoded by genes on chromosomes implicated in 23 inherited cilia-related disorders. Armed with
this knowledge, researchers hope to be able to more quickly find
the exact genetic mutations that cause these 23 cilia diseases,
which include eye and kidney diseases, among others.
Pierce is a pediatric
ophthalmologist who specializes in caring
for children with inherited retinal degenerations. He says that
about half of his patients with degenerative eye diseases have
a type of disease that can be identified according to its genetic
mutation. He believes that this research will help identify the
genetic causes behind the other half of his patients’ conditions.
“We’re narrowing the field,” says Pierce. “This
research in and of itself can’t find a cure, but it’s
a great start because it tells you what proteins to study.”
Co-authors also include Edward
N. Pugh, Jr., from Penn; Glenn Tan,
Natasha
Levenkova, and John
J. Rux, of the Wistar Institute; and
Tiansen
Li of Harvard
Medical School. The National
Eye Institute,
the F.M.
Kirby Foundation, The Foundation
Fighting Blindness, Research
to Prevent Blindness, the Rosanne H. Silbermann Foundation, the
Mackall Foundation Trust, and the Commonwealth University Research
Enhancement Program provided funding for this research.
###
PENN Medicine is a $2.9 billion enterprise
dedicated to the related missions of medical education, biomedical
research, and high-quality patient care. PENN Medicine consists
of the University of Pennsylvania School of Medicine (founded in
1765 as the nation's first medical school) and the University of
Pennsylvania Health System.
Penn's School of Medicine is ranked #2 in the nation for receipt
of NIH research funds; and ranked #3 in the nation in U.S. News
& World Report's most recent ranking of top research-oriented
medical schools. Supporting 1,400 fulltime faculty and 700 students,
the School of Medicine is recognized worldwide for its superior
education and training of the next generation of physician-scientists
and leaders of academic medicine.
The University of Pennsylvania Health System includes three hospitals,
all of which have received numerous national patient-care honors [Hospital
of the University of Pennsylvania; Pennsylvania Hospital, the nation's
first hospital; and Penn Presbyterian Medical Center]; a faculty practice
plan; a primary-care provider network; two multispecialty satellite
facilities; and home care and hospice.
Penn Medicine is one of the world’s leading academic medical centers, dedicated to the related missions of medical education, biomedical research, excellence in patient care, and community service. The organization consists of the University of Pennsylvania Health System and Penn’s Raymond and Ruth Perelman School of Medicine, founded in 1765 as the nation’s first medical school.
The Perelman School of Medicine is consistently among the nation's top recipients of funding from the National Institutes of Health, with $550 million awarded in the 2022 fiscal year. Home to a proud history of “firsts” in medicine, Penn Medicine teams have pioneered discoveries and innovations that have shaped modern medicine, including recent breakthroughs such as CAR T cell therapy for cancer and the mRNA technology used in COVID-19 vaccines.
The University of Pennsylvania Health System’s patient care facilities stretch from the Susquehanna River in Pennsylvania to the New Jersey shore. These include the Hospital of the University of Pennsylvania, Penn Presbyterian Medical Center, Chester County Hospital, Lancaster General Health, Penn Medicine Princeton Health, and Pennsylvania Hospital—the nation’s first hospital, founded in 1751. Additional facilities and enterprises include Good Shepherd Penn Partners, Penn Medicine at Home, Lancaster Behavioral Health Hospital, and Princeton House Behavioral Health, among others.
Penn Medicine is an $11.1 billion enterprise powered by more than 49,000 talented faculty and staff.