It may look like something that belongs in a museum, but the hyperbaric chamber at the Hospital of the University of Pennsylvania has a rich history and continues to provide important treatments for a variety of patients — including those with bone infections, wounds that won’t heal and carbon monoxide poisoning — who benefit from high-pressure oxygen therapy.
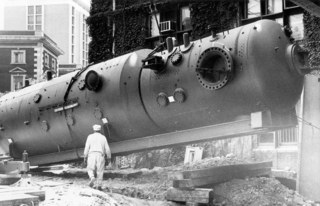 The hyperbaric chamber was first brought to HUP in 1968, and because of its massive size, the building in which it’s housed was then built around it! But the chamber’s story starts even earlier than that… with Christian Lambertsen, MD.
The hyperbaric chamber was first brought to HUP in 1968, and because of its massive size, the building in which it’s housed was then built around it! But the chamber’s story starts even earlier than that… with Christian Lambertsen, MD.
As a graduate student at Penn’s School of Medicine starting in 1939, Lambertsen, founder and former director of Penn’s Institute for Environmental Medicine, was already well on his way to inventing what is known today as SCUBA, or self-contained underwater breathing apparatus. Of note is that Lambertsen’s invention was designed as a closed circuit, where no gas escapes from the system. Modern recreational diving usually uses open systems, where exhaled gas bubbles into the surrounding water. By his second year of medical school, Lambertsen had already published two papers on this groundbreaking research.
Then, in 1941, Lambertsen began working with a branch of the United States Army called the Office of Strategic Services (OSS), a predecessor to what is now known as the Central Intelligence Agency (CIA), which used his invention during World War II as part of its special operational underwater forces. Soon after the war, Lambertsen joined Penn’s faculty and then shortly thereafter the Navy called on him to train their “frogmen,” or combat swimmers, to become divers.
His work with the OSS and the Navy then led Lambertsen to study the physiological effects of pressure, both underwater (hyper) and at high altitudes (hypo) — in other words, how much alteration in pressure the body can sustain — whether that changes in water versus a dry environment, and the dangers of oxygen and carbon dioxide excess. His research utilized healthy volunteers, but more surprisingly, he was often the subject of his own research.
In 1968, the Institute for Environmental Medicine was officially established at Penn, directed by none other than Lambertsen. While the first use for hyperbaric medicine was treating decompression illness resulting from diving or high altitudes, as the Institute evolved, so did the uses for high-pressure oxygen therapy.
“The 1960s marked an evolution from studying oxygen toxicity to utilizing oxygen as a therapy,” said Kevin Hardy, MD, assistant professor of Emergency Medicine and attending physician of Hyperbaric Medicine. Hyperbaric oxygen therapy involves breathing 100 percent oxygen in an elevated pressure environment, which causes up to 20 times more oxygen to travel through the bloodstream to injured organs and tissues. “We’re dosing oxygen like a drug,” said Matthew Kelly, MD, assistant professor of Emergency Medicine and director of clinical services for Hyperbaric Medicine, noting that the air we usually breathe is made up of just 21 percent oxygen.
 Today, Penn’s hyperbaric chamber is mainly used for routine outpatient therapies, often associated with the rare secondary effects of radiation. Basically, since radiation is designed to damage cancer cells, sometimes other cells can become damaged in the process. So, high-pressure oxygen therapy provides an opportunity for new blood vessels to form, in order to heal the damage. A much smaller percentage of those treated are inpatients with a wound or an infection that won’t heal on its own, but the same oxygen therapy healing principles apply.
Today, Penn’s hyperbaric chamber is mainly used for routine outpatient therapies, often associated with the rare secondary effects of radiation. Basically, since radiation is designed to damage cancer cells, sometimes other cells can become damaged in the process. So, high-pressure oxygen therapy provides an opportunity for new blood vessels to form, in order to heal the damage. A much smaller percentage of those treated are inpatients with a wound or an infection that won’t heal on its own, but the same oxygen therapy healing principles apply.
Among the conditions treated with hyperbaric oxygen therapy at HUP are:
- Radiation injury
- Bone infection
- Diabetic and other complex wounds
- Compromised skin grafts or flaps
- Decompression sickness
- Carbon monoxide poisoning
Each day, three scheduled treatments are performed in the hyperbaric chamber, with each treatment typically lasting 100 to 140 minutes and including up to seven patients at a time. A “tender” — often EMT personnel or a paramedic — is present inside the chamber for each treatment (breathing the chamber’s pressurized air, but not wearing a mask delivering oxygen), and an attending physician remains outside the chamber to oversee the treatment. Meanwhile, a smaller chamber remains available for emergency cases.
While hyperbaric medicine is part of the department of Emergency Medicine, it provides a very different experience for physicians and nurses, since they tend to see the same patients for one-week to two-month courses of treatment. “We really get to know the patients and get to see them improve,” said Kelly. “That’s completely different from the emergency room, where patients are in and out, and we never see them again.”
In addition, Penn is one of only eight schools in the country offering a fellowship in Undersea and Hyperbaric Medicine, a point of pride for Hardy, who says, “One main focus of our program is education. We’re turning out board-eligible individuals and creating national leaders in hyperbaric medicine.”
As we celebrate the 250th birthday of the Perelman School of Medicine this year, we look back fondly on the many accomplishments of students and faculty along the way. Lambertsen and his contributions to hyperbaric medicine are a tremendous example of the passion, perseverance and vision that we continue to see from students and faculty today, and look forward to seeing for many years to come.