 The little-known metastatic bile duct cancer—or cholangiocarcinoma—is one of the toughest cancers out there to beat. It’s usually caught late and requires an aggressive round of chemotherapy and radiation that, in most cases, only stabilizes it briefly. It can come roaring back and often leads to death.
The little-known metastatic bile duct cancer—or cholangiocarcinoma—is one of the toughest cancers out there to beat. It’s usually caught late and requires an aggressive round of chemotherapy and radiation that, in most cases, only stabilizes it briefly. It can come roaring back and often leads to death.
But that wasn’t so for a patient at the Abramson Cancer Center, who was the sole focus of a recent report published in ecancer by Arturo Loaiza-Bonilla, MD, an assistant professor in the division of Hematology/Oncology, and Jennifer Morrissette, PhD, clinical director at the Center for Personalized Diagnostics (CPD). She’s a special case. Actually, a more appropriate word would be “exceptional.”
A change in treatment saved her life after a Penn Medicine clinical team performed next-generation DNA sequencing on her tumor, which was growing in the ducts of her liver and metastasizing to the bones and lungs. The tests—developed by and run at Penn’s CPD—take a deeper dive into a patient’s genetic makeup, catching a slew of mutations known to be associated with cancer. In this patient’s case, it found something unexpected—and clinically actionable: BRAF.
We know that the BRAF mutation can be successfully targeted with therapies like vemurafenib or the recently-approved combination of dabrafenib and tramentib. They were originally developed and approved for melanoma; however, physicians have found success in treating other cancers, like lung, colon and most recently thyroid, when patients are found to harbor the mutation. But cholangiocarcinoma?
The patient underwent treatment immediately, and the primary tumor quickly shrunk. Over time, the cancer in the other parts of her body responded well to the treatments, and today, the patient is almost completely asymptomatic and nearly deemed cancer free.
“This was the first reported case of the use of personalized genomic information for the successful management of a patient with cholangiocarcinoma, and it is also the first description of BRAF-targeted therapy in this cancer,” Loaiza-Bonilla said. “This is what we call an ‘exceptional response,’ and it’s providing the foundation for future clinical studies on this cancer and even other malignancies. Let’s learn more about this response and find others who may benefit as well.”
Stories of these “exceptional responders” continue to surface in journal and newspaper articles, but it’s often the other way around, where a very select few of patients do well on a treatment, while most others fail. And no one knows exactly why.
Another Abramson Cancer Center patient, who was the subject of Bloomberg article this past spring, is a prime example. In 2009, 29 patients with advanced melanoma were enrolled in an experimental immunotherapy drug trial, but the 70-year-old grandmother was the only one who went into remission. Now, she is part of a genomic analysis at Penn’s CPD to see exactly why she responded so well.
That’s also the goal of the newly announced National Cancer Institute Exceptional Responder Initiative. The project aims to collect samples from at least 100 of these “exceptional responders” around the country, and mine their genes for valuable information that could reveal clues about treating others.
Scientists will attempt to identify the molecular features in tumors that predict whether or not a particular drug will be beneficial. Investigators will examine tumor specimens from patients in clinical trials who achieved an exceptional response relative to other trial participants.
Matching patients with existing therapies designed to target mutations previously associated only with different cancers is also one of the main goals of Penn Medicine’s CPD, where over 2,500 tumors from patients have been sequenced so far.
“Our cholangiocarcinoma case and other experiences of ‘extraordinary responders’ can all teach us something and help unravel some of the genetic mysteries of cancers,” said Loaiza-Bonilla. “They also stress the importance of taking a personalized approach to cancer, with a multidisciplinary molecular tumor board to critically analyze a patient’s mutations and options.
“As more data surfaces and patients’ tumors are sequenced, such an approach will likely transform the treatment paradigm in oncology.”
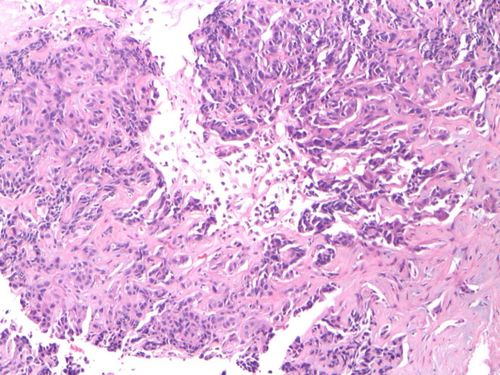
Photo credit: High-power magnification of a cholangiocarcinoma tumor. Loaiza-Bonilla et al. ecancer. November 2014.