Magnetic resonance imaging (MRI) provides exquisite structural detail of the brain. However, current MRI methods can't image the detailed distribution of neurotransmitters – the brain’s chemical messengers -- across the whole brain.
Current imaging techniques for glutamate, a major neurotransmitter, is anything but perfect, but it still lets physicians and researchers gain fleeting glimpses into one of biology’s greatest mysteries: the inner workings and connectivity of the human brain.
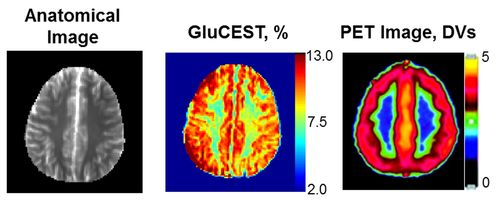
A new Nature Medicine paper out this week from Perelman School of Medicine researchers led by Ravinder Reddy, PhD, professor of Radiology, describes a first-of-its-kind MRI technique (GluCEST) to measure glutamate concentration and local changes across the whole brain. The technique is based on chemical exchange effects on water proton MRI.
While other MRI methods, such as functional MRI (fMRI) and ASL, provide information about brain function and blood perfusion, they are not capable of measuring glutamate changes.
Glutamate is involved in most disorders of the central nervous system, so neurologists and radiologists have been searching for imaging techniques that would allow them to see the distribution of glutamate across the entire brain at high resolution. This would allow them to compare details in neurotransmitter concentration from one brain region to the next. For example, in Alzheimer’s disease (AD), patients’ glutamate concentration decreases in affected parts of the brain compared to control subjects without symptoms of AD. Conversely, glutamate concentration increases in epileptic patients in some brain regions compared to controls.
For now, glutamate is imaged two ways in live brains. First is proton magnetic resonance spectroscopy, which only gives views of local regions of the brain, such as the hippocampus. The second is positron emission tomography (PET), which also has spatial resolution limitations, and involves small amounts of radiation.
“It’s the changes in glutamate that are important to measure and compare, on a whole-brain scale, says senior author Reddy.
When comparing this new method with PET in scans of healthy human brains, the team saw more details in the landscape of white matter and gray matter in the whole brain using the GluCEST method.
GluCEST is also extremely sensitive to changes in pH in microenvironments surrounding tissues. Because tissue pH changes may trigger many pathological processes, a noninvasive technique to image pH may provide new avenues for early detection of disease as well as response to treatment. For example, in a brain that has suffered a stroke, the immediately affected regions have a low pH. Tissue at different distances away from the site are more or less acidic, and therefore more or less salvageable.
A map of the pH gradient around stroke-affected tissue would help physicians better direct treatment. With further studies on preclinical models and appropriate calibrations it may be possible to use this method to map the pH changes. Future studies using this approach may provide new insights into glutamate function and demonstrate its potential as a biomarker for the diagnosis and treatment of many types of neurological disorders.
This project was supported by the National Center for Research Resources and the National Institute of Biomedical Imaging and Bioengineering of the National Institutes of Health through Grant Number BTRC P41EB015893.
Read More
 Cai, K., Haris, M., Singh, A., Kogan, F., Greenberg, J., Hariharan, H., Detre, J., & Reddy, R. (2012). Magnetic resonance imaging of glutamate Nature Medicine DOI: 10.1038/nm.2615
Cai, K., Haris, M., Singh, A., Kogan, F., Greenberg, J., Hariharan, H., Detre, J., & Reddy, R. (2012). Magnetic resonance imaging of glutamate Nature Medicine DOI: 10.1038/nm.2615