Clinical departments at HUP are re-imagining what health care can and should look like. Some changes, such as properly spaced seats and readily available hand sanitizer in the waiting area, are new in response to new safety needs of the COVID-19 pandemic. But for Women’s Health, which will undergo significant changes at HUP West once the Pavilion (HUP East) opens, big plans were already underway, and continue, to change health care delivery for the better.
Here’s how they’re doing it.
A Unique Approach to Solving Problems
“What must we do starting now and over the next two years to design and create the ideal experiences and environments to advance high-value patient and family-centered women’s health care at HUP?”
That was the question that a group of 27 participants — representing a wide variety of stakeholders in Women’s Health at HUP — were brought together to answer last fall. They listened to what each considered his or her most important issues surrounding the question and together narrowed a long list into a set of strategies and actions that would lead them to their goal... all within two days. This is Syntegration.
In reimaging Women’s Health, everything is being examined, from the actual physical layout—making sure there’s close proximity among all of the units — to the kind of technology necessary to bring new innovations to patient care, for example, the Healing at Home pilot which provides 24/7 text support to moms who are able to leave the hospital a day early after a normal vaginal birth.
Typically, in making these kinds of plans, a small group collects feedback from stakeholders and then decides the best direction to take; the individual groups rarely talk with each other about things that are important to them. In Syntegration, stakeholders actually talk with one another — thousands of person-to -person interactions called collisions — to help them come up with the final plans of action, based on what they all consider important.
“This brought stakeholders together with different perspectives — you hear their ideas directly, what’s on top of their minds,” said Deborah Driscoll, MD, SVP for the Clinical Practices of the University of Pennsylvania and former chair of OB/GYN.
Also, unlike the traditional process using consultants, results do not take months or even weeks. Plans of action are created within days. “It’s a rigorous time frame but the effort doesn’t lose momentum,” said Regina Cunningham, PhD, RN, HUP’s CEO. “It’s efficient and keeps people engaged.”
Ready, Set … Go!
When it came to choosing participants for the Syntegration workshop, people from both clinical and nonclinical areas were selected. “We were looking for people who were willing to speak up and think creatively about the future,” Driscoll said.
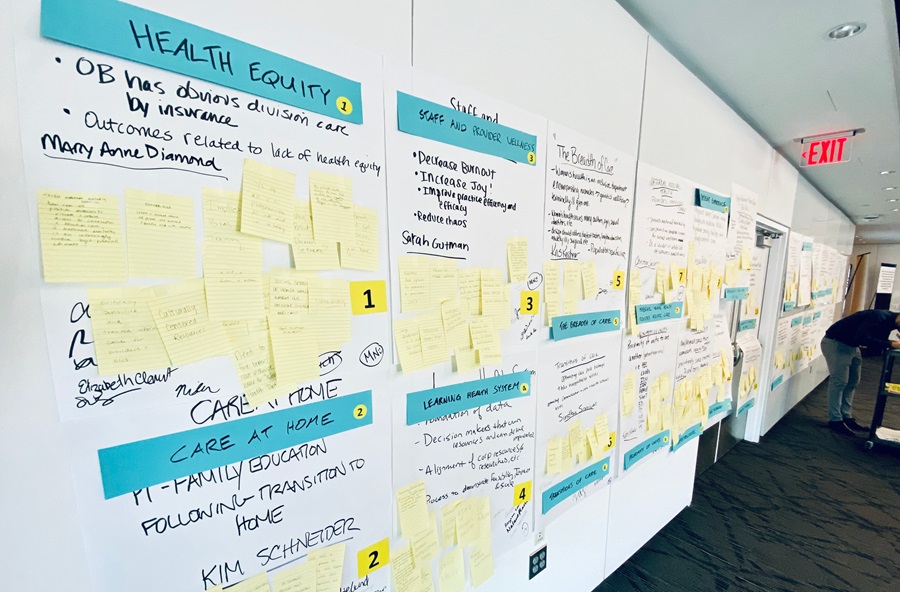
The planning session kicked off with a wall full of stickies — over 400! — representing “statements of importance,” that is, what each participant felt was crucial to consider in moving ahead. For example, make sure all services are in one space or retaining the right staff. Working with Syntegrity facilitators, the group combined similar ideas and narrowed the suggestions down to eight specific topic areas. This set the agenda to be discussed in three rounds of meetings held over the next day and a half.
For each of the meetings, each participant was assigned a role, and different groups of people were brought together in one of the three roles. “Members” drove the conversation at each round. “Critics” were not part of the actual discussion but provided feedback as to how they thought the conversation was proceeding. “It was not criticism of the thoughts or ideas, but of the conversation itself. What is missing from the conversation?” said Jessica Lazzeri, MSN, clinical director of Women’s Health. “Observers” listened and took notes. At the end of the three meetings, participants narrowed the ideas down to three specific recommendations to help each of the eight topics move forward.
What Comes Next?
In the final part, using fake money, each person “invested” in the recommendations they considered priorities to help Women’s Health reach its goal over the course of the next two years. This resulted in a list of 10 projects.
While Driscoll had expected to see the use of technology, innovation, etc. in delivering better care on the list, “what also emerged was a focus on disparities in health care, integrating behavioral health and using data to inform our decisions,” Driscoll said. “I hadn’t expected that. That’s what’s unique about this process.”
Following the workshop, a team was created for each topic, tasked with bringing “all the things we envisioned to fruition over the next two years,” Cunningham said. In the wake of the pandemic, the work of the Syntegrity teams was put on hold, but Lazzeri said that plans to decide the best way to move forward are being discussed. In the meantime, the response to the COVID-19 pandemic has itself prompted other changes and plans for the future of Women’s Health.
The mental and behavioral impact of COVID-19 has made behavioral health resources in the new Women’s Health especially crucial. “We have already started collaborating with Psychiatry to develop a systematic, integrated approach that allows us to provide greater access and a shared approach to the mental health needs of our patients,” said Sindhu Srinivas, MD, director of Obstetrical Services at HUP.
Samuel Parry, MD, interim chair of OB/GYN, said that COVID-19 has made telemedicine a definite part of medicine’s future. As a result, in planning Women’s Health’s expanded space in HUP West, “there will need to be dedicated space in a quiet area and dedicated computers,” he said. While not every OB/GYN condition can be seen via telemedicine, many readily lend themselves to a virtual visit, including postpartum visits or a discussion of contraception options.